◔
CRPS: Difference between revisions
From WikiMSK
m (Text replacement - "Hand & Wrist" to "Hand and Wrist") |
No edit summary |
||
| Line 4: | Line 4: | ||
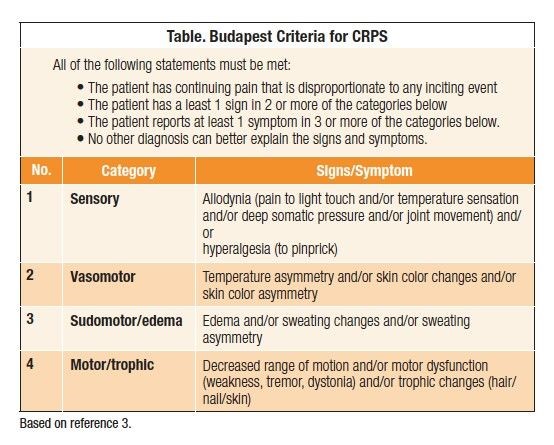
===Budapest Criteria=== | ===Budapest Criteria=== | ||
[[File:Budapest Criteria.jpg|554px]] | [[File:Budapest Criteria.jpg|554px]] | ||
== Management == | |||
=== Principles === | |||
The four pillars of management : | |||
# Patient information and education to support self-management. | |||
# Pain relief (medication and procedures). | |||
# Psychosocial and behavioural management. | |||
# Physical and vocational rehabilitation ( and activities of daily living and societal participation) . | |||
A coordinated Multidisciplinary Program should therefore involve: | |||
* Education | |||
* Medical | |||
* Physiotherapy and OT | |||
* Psychological and Behavioural | |||
* Societal and Vocational | |||
Vocational and litigation support may be provided by specialist rehabilitation teams and, in other cases, these services are integrated into the regional pain management programme | |||
* Active engagement of the patient/family in goal setting, goal review | |||
* Control | |||
** the patient remains responsible for their own rate of progress. | |||
* Understanding and insight: | |||
** how emotional stress, muscle tension and de-conditioning can increase pain experience. | |||
** how their own behaviours may serve to exacerbate pain experience. | |||
* Learning: | |||
** self-management approach, including goal setting and pacing. | |||
** the right balance between doing too much and too little. | |||
** relaxation techniques, breathing exercises etc to reverse sympathetic arousal. | |||
* Empowering the family: | |||
** encouraging individual to keep active | |||
=== Medical Management === | |||
Investigation and confirmation of diagnosis: | |||
* Pharmacological intervention (in conjunction with pain team wherever appropriate) to provide a window of pain relief. | |||
* Reassurance that physical and occupational therapy are safe and appropriate. | |||
* Provide medical follow-up to prevent iatrogenic damage through inappropriate referral. | |||
* Support any litigation/compensation claim to its resolution and conclusion.(if desired and appropriate). | |||
=== Psychosocial and Behavioural management === | |||
* Identify any psychological factors contributing to pain and disability. | |||
* Treat anxiety and depression. | |||
* Identify, explore and proactively address any internal factors (eg counter-productive behaviour patterns)or external influences (eg. perverse incentives, family dynamics etc) which may perpetuate disability/dependency. | |||
* Consider needs of family/carers – provide psychological intervention/counselling where appropriate. | |||
* Provide a practical problem-solving, goal-orientated approach (involving both the patient and their family) to reduce barriers and promote healthy functioning. | |||
=== Physical management === | |||
Retrain normal body posture. | |||
* Desensitisation – handling the affected part followed by passive stretching/isometric exercise. | |||
* Progression to active isotonic exercise and then strength training. | |||
* General body re-conditioning – cardiovascular fitness. | |||
* Encourage recreational physical exercise and functional goals. | |||
* Techniques to address altered perception and awareness of the limb, eg. mirror visual feedback training or graded motor imagery. | |||
=== Activities of daily living and societal participation === | |||
* Support graded return to independence in activities of daily living with clear functional goals. | |||
* Assessment and provision of appropriate specialist equipment/adaptations to support independence. | |||
* Removal of inappropriate/unnecessary equipment. | |||
* Adaptation of environment. | |||
* Extend social and recreational activities in and outside the home. | |||
* Workplace assessment/vocational re-training. | |||
==Videos== | ==Videos== | ||
| Line 9: | Line 76: | ||
==Article Downloads== | ==Article Downloads== | ||
[[ | [[Media:Harden2010_-_Budapest_Criteria.pdf]] | ||
==References== | ==References== | ||
Revision as of 12:46, 17 July 2021
This article is a stub.
Diagnosis
Budapest Criteria
Management
Principles
The four pillars of management :
- Patient information and education to support self-management.
- Pain relief (medication and procedures).
- Psychosocial and behavioural management.
- Physical and vocational rehabilitation ( and activities of daily living and societal participation) .
A coordinated Multidisciplinary Program should therefore involve:
- Education
- Medical
- Physiotherapy and OT
- Psychological and Behavioural
- Societal and Vocational
Vocational and litigation support may be provided by specialist rehabilitation teams and, in other cases, these services are integrated into the regional pain management programme
- Active engagement of the patient/family in goal setting, goal review
- Control
- the patient remains responsible for their own rate of progress.
- Understanding and insight:
- how emotional stress, muscle tension and de-conditioning can increase pain experience.
- how their own behaviours may serve to exacerbate pain experience.
- Learning:
- self-management approach, including goal setting and pacing.
- the right balance between doing too much and too little.
- relaxation techniques, breathing exercises etc to reverse sympathetic arousal.
- Empowering the family:
- encouraging individual to keep active
Medical Management
Investigation and confirmation of diagnosis:
- Pharmacological intervention (in conjunction with pain team wherever appropriate) to provide a window of pain relief.
- Reassurance that physical and occupational therapy are safe and appropriate.
- Provide medical follow-up to prevent iatrogenic damage through inappropriate referral.
- Support any litigation/compensation claim to its resolution and conclusion.(if desired and appropriate).
Psychosocial and Behavioural management
- Identify any psychological factors contributing to pain and disability.
- Treat anxiety and depression.
- Identify, explore and proactively address any internal factors (eg counter-productive behaviour patterns)or external influences (eg. perverse incentives, family dynamics etc) which may perpetuate disability/dependency.
- Consider needs of family/carers – provide psychological intervention/counselling where appropriate.
- Provide a practical problem-solving, goal-orientated approach (involving both the patient and their family) to reduce barriers and promote healthy functioning.
Physical management
Retrain normal body posture.
- Desensitisation – handling the affected part followed by passive stretching/isometric exercise.
- Progression to active isotonic exercise and then strength training.
- General body re-conditioning – cardiovascular fitness.
- Encourage recreational physical exercise and functional goals.
- Techniques to address altered perception and awareness of the limb, eg. mirror visual feedback training or graded motor imagery.
Activities of daily living and societal participation
- Support graded return to independence in activities of daily living with clear functional goals.
- Assessment and provision of appropriate specialist equipment/adaptations to support independence.
- Removal of inappropriate/unnecessary equipment.
- Adaptation of environment.
- Extend social and recreational activities in and outside the home.
- Workplace assessment/vocational re-training.
Videos
Article Downloads
Media:Harden2010_-_Budapest_Criteria.pdf
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,