◒
De Quervain Injection: Difference between revisions
From WikiMSK
| (32 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
|syringe=1mL | |syringe=1mL | ||
|needle=25G 16mm | |needle=25G 16mm | ||
|steroid= | |steroid=0.5mL 20mg triamcinolone | ||
|local=0. | |local=0.5mL 1% lidocaine | ||
|volume=1mL | |volume=1mL | ||
}} | }} | ||
| Line 13: | Line 13: | ||
==Anatomy== | ==Anatomy== | ||
The APL and EPB usually run together in the first dorsal compartment. The tendons can often be seen with the thumb held in resisted extension. They can also be palpated at the base of the 1st metacarpal. | [[File:De Quervain Compartments.PNG|200px|thumb|A. One compartment.<br/>B. Two subcompartments<br/>From McDermott et al 2012<ref>McDermott JD, Ilyas AM, Nazarian LN, Leinberry CF. Ultrasound-guided injections for de Quervain's tenosynovitis. Clin Orthop Relat Res. 2012;470(7):1925-1931. doi:10.1007/s11999-012-2369-5</ref>]] | ||
*The APL and EPB usually run together in the first dorsal compartment. | |||
*The tendons can often be seen with the thumb held in resisted extension. | |||
*They can also be palpated at the base of the 1st metacarpal. | |||
*Anatomic variation: septum with two sub compartments (24-76% in cadaver studies). Failure can occur if failure to inject into compartment or only one sub compartment. | |||
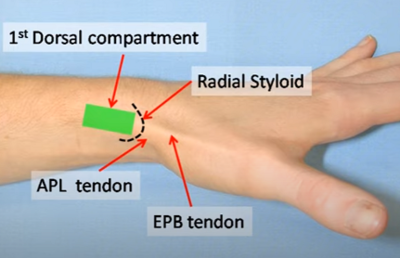
[[File:First Dorsal Compartment.PNG|400px]] | |||
==Indications== | |||
==Contraindications== | |||
==Technique== | ==Technique== | ||
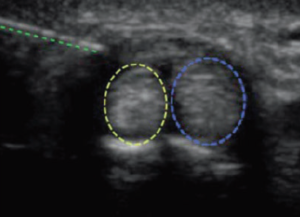
* | [[File:De Quervain Ultrasound Injection.PNG|300px|thumb|Long axis injection. From left to right: needle, EPB, APL.]] | ||
*Ultrasound guided is preferred with greater clinical improvement, and allows the identification of subcompartment anatomical variation <ref>McDermott JD, Ilyas AM, Nazarian LN, et al. Ultrasound-guided injections for de Quervain's tenosynovitis. Clin Orthop Relat Res. 2012;470:1925–31.</ref><ref>Jeyapalan K, Choudhary S. Ultrasound-guided injection of triamcinolone | |||
and bupivacaine in the management of de Quervain’s disease. Skelet Radiol. 2009;38:1099–103.</ref><ref>Zingas C, Failla JM, Van Holsbeeck M. Injection accuracy and clinical | |||
relief of de Quervain’s tendinitis. J Hand Surg Am. 1998;23:89</ref> | |||
*Position: Ulnar side of hand resting on surface with thumbheld in slight flexion | *Position: Ulnar side of hand resting on surface with thumbheld in slight flexion | ||
*Identify the gap between the two tendons | |||
===Non-Ultrasound Guided=== | |||
*Identify: Radial styloid, the APB and EPL tendons, and the gap between them. | |||
*Injection site | |||
** Usual site: is between 5-10mm proximal to the tip of the radial styloid, between the two tendons, through the retinaculum, within the sheath. | |||
** Alternative site in very thin patients: inject distal to the retinaculum, 5mm distal to the radial styloid (due to limited subcutaneous tissue), then advance the needle proximally while injecting | |||
*Insert needle perpendicularly into the gap then slide proximally between the tendons (needle going distal to proximal) | *Insert needle perpendicularly into the gap then slide proximally between the tendons (needle going distal to proximal) | ||
*Inject solution as a bolus | *Inject solution as a bolus | ||
===Ultrasound Guided=== | |||
* Preparation: Stand off gel recommended | |||
* Identify: APL and APB tendons in sagittal, retinaculum, radial styloid in transverse | |||
* Optional: initial infiltration of lidocaine. | |||
* Axis: Can be done long axis or short axis. Transverse view is best with the needle entering the sheath while in plan with the transducer. | |||
* Direction: Dorsal to palmar direction, at a site free of superficial veins and the superficial branch of the radial nerve | |||
* Injection | |||
**One sheath: deposit at one location in the sheath | |||
**Two sheaths: Pierce the septum between the sheaths. Deposit half around the APL, then draw back and deposit the remaining half around the EPB | |||
==Complications== | ==Complications== | ||
*Subcutaneous fat atrophy, particularly noticeable in dark skinned thin women. This may be permanent. The risk can be reduced by using hydrocortisone. | *Subcutaneous fat atrophy, particularly noticeable in dark skinned thin women. This may be permanent but generally resolves within 3 months. The risk can be reduced by using hydrocortisone. | ||
*Trauma to superficial radial nerve | *Trauma to superficial radial nerve | ||
| Line 29: | Line 59: | ||
Rest hand for one week with taping. Avoid provoking activities and start a graded load programme. | Rest hand for one week with taping. Avoid provoking activities and start a graded load programme. | ||
== | ==External Resources== | ||
<youtube>Y8BSLvsyRTg</youtube> | <youtube>Y8BSLvsyRTg</youtube> | ||
[[Category:Hand | {{PDF|McDermott2012 Ultrasound guided de Quervain injection.pdf|Ultrasound guided de Quervain Injection - McDermott 2012}} | ||
[[Category: | |||
==References== | |||
<references/> | |||
{{Reliable sources}} | |||
[[Category:Hand and Wrist Procedures]] | |||
[[Category:Infoboxes]] | |||
[[Category:Partially complete articles]] | |||
Latest revision as of 14:21, 16 March 2022
This article is still missing information.
| De Quervain Injection | |
|---|---|
| Indication | De Quervain Tendinopathy |
| Syringe | 1mL |
| Needle | 25G 16mm |
| Steroid | 0.5mL 20mg triamcinolone |
| Local | 0.5mL 1% lidocaine |
| Volume | 1mL |
Background
Injection for De Quervain Tendinopathy.
Anatomy
- The APL and EPB usually run together in the first dorsal compartment.
- The tendons can often be seen with the thumb held in resisted extension.
- They can also be palpated at the base of the 1st metacarpal.
- Anatomic variation: septum with two sub compartments (24-76% in cadaver studies). Failure can occur if failure to inject into compartment or only one sub compartment.
Indications
Contraindications
Technique
- Ultrasound guided is preferred with greater clinical improvement, and allows the identification of subcompartment anatomical variation [2][3][4]
- Position: Ulnar side of hand resting on surface with thumbheld in slight flexion
Non-Ultrasound Guided
- Identify: Radial styloid, the APB and EPL tendons, and the gap between them.
- Injection site
- Usual site: is between 5-10mm proximal to the tip of the radial styloid, between the two tendons, through the retinaculum, within the sheath.
- Alternative site in very thin patients: inject distal to the retinaculum, 5mm distal to the radial styloid (due to limited subcutaneous tissue), then advance the needle proximally while injecting
- Insert needle perpendicularly into the gap then slide proximally between the tendons (needle going distal to proximal)
- Inject solution as a bolus
Ultrasound Guided
- Preparation: Stand off gel recommended
- Identify: APL and APB tendons in sagittal, retinaculum, radial styloid in transverse
- Optional: initial infiltration of lidocaine.
- Axis: Can be done long axis or short axis. Transverse view is best with the needle entering the sheath while in plan with the transducer.
- Direction: Dorsal to palmar direction, at a site free of superficial veins and the superficial branch of the radial nerve
- Injection
- One sheath: deposit at one location in the sheath
- Two sheaths: Pierce the septum between the sheaths. Deposit half around the APL, then draw back and deposit the remaining half around the EPB
Complications
- Subcutaneous fat atrophy, particularly noticeable in dark skinned thin women. This may be permanent but generally resolves within 3 months. The risk can be reduced by using hydrocortisone.
- Trauma to superficial radial nerve
Aftercare
Rest hand for one week with taping. Avoid provoking activities and start a graded load programme.
External Resources
References
- ↑ McDermott JD, Ilyas AM, Nazarian LN, Leinberry CF. Ultrasound-guided injections for de Quervain's tenosynovitis. Clin Orthop Relat Res. 2012;470(7):1925-1931. doi:10.1007/s11999-012-2369-5
- ↑ McDermott JD, Ilyas AM, Nazarian LN, et al. Ultrasound-guided injections for de Quervain's tenosynovitis. Clin Orthop Relat Res. 2012;470:1925–31.
- ↑ Jeyapalan K, Choudhary S. Ultrasound-guided injection of triamcinolone and bupivacaine in the management of de Quervain’s disease. Skelet Radiol. 2009;38:1099–103.
- ↑ Zingas C, Failla JM, Van Holsbeeck M. Injection accuracy and clinical relief of de Quervain’s tendinitis. J Hand Surg Am. 1998;23:89
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,