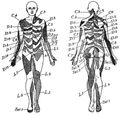
Dermatomes
The most up to date dermatome map is probably that published by Lee et al. They created a composite image taken from published data that they thought was the most reliable. [1] The winding band like dermatomal map seen in some textbooks was from Keegan and Garrett is the most flawed of all dermatomal maps and was not included. Lee et al's map is most consistent tactile dermatomal regions for each spinal dorsal nerve root. The midline has minimal overlap, but otherwise there is extensive and variable overlap. Blank areas on the map represent areas where there is very large degree of variability and overlap. The S3, S4, and S5 cutaneous supply is not shown.
Radicular pain does not necessarily follow dermatomal distribution.[2]
History
See Downs et al on the history of dermatome maps.[3]
| Authors | Year | Basis of Map | Findings | Weaknesses |
|---|---|---|---|---|
| Herringham | 1886 | The first account of the distribution of segmental nerve fibres into the upper limb based on dissection | Axial line. The dermatomes in the preaxial area (C5-6) are higher than those in the post axial area (C8-T1). In the preaxial area the forearm (C6) is supplied by a lower nerve than the arm (C5), in the post axial area the forearm (C8) is supplied by a higher nerve than the arm (T1-2) | Only based on dissection and theory. |
| Sherington | 1893 | Severing dorsal nerve roots in monkeys and testing sensation, distributions drawn on a plaster cast of a monkey. | Adjacent dermatomes overlap, except for proximal aspects of the limbs. Nerve fibre density is lower towards the periphery of a dermatome | Animal based study |
| Head and Campbell | 1900 | Zoster eruptions in 450 patients, with histological confirmation in some subjects. | Noted some overlap, changed with body shape and age. Uniquely studied the thoracic dermatomes. | Histological confirmation in only 16 cases. No examples of C8 or S1. Assumptions were made about the exact dorsal root involved. Herpetic eruptions can affect several adjacent levels. Not all cutaneous fibres will necessarily be infected. |
| Fender and Foerster | 1933 and 1936 | Residual area of sensation after surgically isolating single dorsal nerve roots. L1 to S2 isolated by dividing nerve roots above and below the target level. Cervical dermatomes mostly assessed by dividing nerve roots either above or below thus obtaining proximal and distal boundaries only. Vasodilation following electrical stimulation supplemented the data. Population those with spasticity (mostly those with tabes dorsalis). | Areas vary between individuals, except in the midline. Tactile dermatomes are larger than those determined by pain and temperature. With the exception of C2 there is no sensory loss if only one nerve root is sectioned. | Relatively few subjects, poorly documented methods and testing protocol, no information about time interval between sectioning and testing. |
| Keegan and Garrett | 1948 | Diminished cutaneous sensitivity of "light pin-scratch" from disc prolapse causing nerve root compression, majority confirmed by myelography, some confirmed surgically. 165 prolapses at C5-T1. 1264 prolapses at L3-S2. Supplemented with nerve root sectioning in 13, and radiologically guided local anaesthetic injection into lower cervical nerve roots in 10 medical students. | Neat nonoverlapping bands running down the limbs from the posterior midline. They acknowledged that the mapping did not represent the complete distribution and dermatomes do overlap. They disputed Foerster on the findings of division of a single nerve root not causing diminished sensation. | The most flawed of the three core maps. Their findings have never been replicated. Some dermatomes not assessed but appear in chart (e.g. L1 and L2, and truncal dermatomes). They reported that the area of hypoalgesia was reproducible and non-variable which differs from other reports. Does not fit with our embryological understanding. Predates our understanding of how disc prolapse in one segment can cause compression of the traversing nerve root, this will not have been picked up on myelography. Doesn't take into account compression of multiple nerve roots. |
| Davis et al | 1952 | 500 patients with disc prolapse mostly L4-5 and L5-S1, verified by myelography and surgery. Sensory changes mapped by independent assessors with light touch and pin prick. | Areas of sensory loss of L5 and S1 very variable between subjects, and there was also variation between assessors. They did not find narrow bands of hypo-aesthesia like Keegan and Garrett. Half of the patients had sensory changes of the foot and leg only. Thought variability related to extent and location of herniated disc | |
| Lee et al | 2008 | Redrew the Head and Campbell, and Foerster maps from the original photographs onto a figure outline. The figures were overlaid, and the areas that did not overlap were deleted. This new template was then modified in the light of other good category evidence data for C6, C7, and C8 (Inouye and Buchthal, 1977) and L4, L5, and S1 (Cole et al., 1968; Nitta et al., 1993). | The lumbosacral variability is greater than cervical. Adjacent dermatomes overlap to a variable degree. Dermatomes in the hand overlap to a large degree. Variability may be explained by the following reasons. Almost all areas of the skin are supplied by two or more spinal nerve roots. Intrathecal intersegmental anastamoses are common. The distribution of a dorsal root is slightly different to that of a dorsal root ganglion, and these areas are influenced by spinal cord processing. Dermatomes vary based on the method of assessment, the type of sensation tested, and the precise neural element being tested | No independent data |
Videos
- ↑ Lee et al.. An evidence-based approach to human dermatomes. Clinical anatomy (New York, N.Y.) 2008. 21:363-73. PMID: 18470936. DOI.
- ↑ Furman & Johnson. Induced lumbosacral radicular symptom referral patterns: a descriptive study. The spine journal : official journal of the North American Spine Society 2019. 19:163-170. PMID: 29800710. DOI.
- ↑ Downs & Laporte. Conflicting dermatome maps: educational and clinical implications. The Journal of orthopaedic and sports physical therapy 2011. 41:427-34. PMID: 21628826. DOI.