Diffuse Idiopathic Skeletal Hyperostosis
Diffuse idiopathic skeletal hyperostosis (DISH) is a noninflammatory condition causing calcification and ossification of spinal ligaments and entheses. It is also known as ankylosing hyperostosis, Forestier disease, and Forestier-Rotes-Querol disease. The condition may be asymptomatic, or may be associated with spinal pain.
Aetiology
The cause of DISH is unknown, however it has been thought that certain factors may be important in its development. These include mechanical factors, diet, drugs, environmental exposures, and metabolic conditions. It is thought that there is abnormal osteoblastic differentiation and activity located at the entheses, as some patients may be deficient in certain inhibitors of bone formation such as Dickkopf-1 and matrix Gla protein.
- Mechanical factors
A right-sided prominence of bony bridging is seen at the thoracic spine. There may be mechanical factors associated with the location of the aorta. Interestingly, in those with dextrocardia or situs inversus, the bony bridging is more prominent on the left.
Mechanical forces may affect bone formation. In those with ossification of the posterior longitudinal ligament (may occur with DISH or independently), ligamentous stretching can increase prostaglandin I2 synthase which results in stimulation of osteogenic differentation. Dickkopf-1, an inhibitor of osteoblastogenesis, may be reduced in those with DISH thereby promoting hyperostosis.
There does not appear to be a difference in the amount of heavy work done in those with DISH compared to controls.
- Environmental factors and diet
Fluoride has been investigated but found unlikely to be a cause. There are mixed reports of the association between higher serum retinol (signifying excessive vitamin A exposure) levels and DISH.
- Medications
Isotretinoin, which is a derivative of vitamin A, and other retinoids are associated with hyperostosis, but more-so in extraspinal areas.
- Metabolic conditions
It is thought that metabolic factors many contribute to increased osteoblastic activity in DISH. Some studies report increased levels of insulin, insulin-like growth factor 1, and growth hormone. Insulin-like growth factor 1 stimulates osteoblasts, and growth hormone can increase the production of this factor.
There are some intriguing demographic studies looking at the association between DISH and metabolic conditions. The Pima Native American people have both a high incidence of DISH and metabolic conditions such as obesity, hypertension, diabetes mellitus, and hyperinsuliaemia. DISH appears to be more common in obese Caucasian people, and possibly also in those with diabetes mellitus. DISH is also seen in up to 20 percent in acromegalic patients.
Also seen in the condition is increased vascularity of the ossified ligaments. It is not known whether this is a cause or a downstream effect of DISH.
Other factors have been studied in their role in DISH. Platelet-derived growth factor-BB and transforming growth factor-1-beta in the cells of ligaments can increase levels of nuclear factor kappa B. Nuclear factor kappa B can promote osteoblastogenesis. Curiously, there are elevated levels of matrix Gla in DISH, but this protein is thought to inhibit bone formation.
Epidemiology
DISH is more common in men than woman, and it is rare under the age of 40.
There are some demographic variations. In Japan, ossification of the posterior longitudinal ligament, mainly in the cervical spine, is 80 time more common than in Europe at 4%. American blacks have lower levels of DISH than whites. The Pima Native American people can develop DISH young, rising to 48% in men and 12% in women in those over 55 years old. In Finland the prevalence is 3.8% in men and 2.6% in women in those over 40. In Hungary the prevalence is 4.9% in men and 1.4% in women over age 50. Studies done in hospitals find a higher prevalence of DISH than the general population.
Clinical Features
Patients with DISH may have pain in the neck, thoracic spine, low back, and/or the extremities. Thoracic spine involvement is present universally in advanced cases, and typically involves T7-T11. There may be reduced spinal mobility. Myelopathy has been reported to occur in some individuals. Dysphagia and airway obstruction can also occur. It is unclear whether it is associated with other musculoskeletal or systemic diseases. Most studies on clinical features are done in patients seen in clinics and the hospital, and so are more likely to have symptoms.
- Musculoskeletal manifestations
Morning spinal stiffness is present in around 80% of individuals, which is a symptoms normally associated with inflammatory conditions. Higher pain levels are seen in those with DISH compared to "lumbar spondylosis" and healthy controls. Disability scores are also higher in DISH compared to healthy controls, and patients may reports difficulty bending and having weak grip strength. Men are less likely to complete five chair stands without using their arms.
Radicular pain and lumbar spinal stenosis are not a typical features of DISH, and if present it may be unrelated.
Pain in the thoracic spine is the most common symptoms and occurs in 40 to 80% of subjects. Pain in the extremities and dysphagia are less common, reported in 15 to 25%. Stridor is a rare symptom resulting from large C2 to C3 anterior osteophytes. This may cause odynophagia and otalgia due to hypopharyngeal ulceration from the pressure. There is an increased risk of dysphagia, due to compression of the oesophagus from anterior cervical osteophytes. Other manifestations of cervical disease are hoarseness, aspiration pneumonia, sleep apnoea, atlantoaxial subluxation or pseudoarthrosis, and thoracic outlet syndrome.
There are mixed reports on the association between radiologic findings and symptoms at that site. There appears to be a significant association between shoulder hyperostosis and shoulder symptoms, as well as a non-significant association between elbow hyperostosis and elbow symptoms. Meanwhile there is no apparent link between spinal hyperostosis and spinal pain. In those with DISH and chronic low back pain, there is also a non-significant increase in media epicondylitis, knee enthesitis, plantar fasciitis, and dysphagia, compared to patients with "lumbar spondylosis."
- Neurological manifestations
Ossification of the posterior longitudinal ligament (OPLL) can cause spinal cord compression and myelopathic symptoms. This appears to be more common in Asian people. Some patients have developed tetraparesis and tetraplegia. Symptoms of cervical myelopathy development that should alert the clinican are a sharp, shoorting neck pain, sudden loss of neck range of motion, unsteady gait and hyperreflexia, and new extremity sensory symptoms.
Other rare findings are horner's syndrome, recurrent laryngeal nerve palsy, and vertebral artery insufficiency.
Examination
Physical examination may reveal decreased spinal range of motion, especially in the thoracic spine. Typically there is a loss of thoracic lateral flexion. There may be nodules palpable at the enthesis. The most common sites of these nodules are the Achilles, knee, and elbow.
There appears to be an increased rate of Bouchard and Heberden nodes in those with DISH.
Radiological findings
Radiological manifestations are the hallmark of DISH, characterised by ossification of the paravertebral ligaments and peripheral entheses.
Spinal Inolvement
See articles on radiopaedia.org for copious examples of DISH and OPLL
The thoracic spine is the most commonly affected, but there may also be abnormalities in the cervical spine, lumbosacral spine, and extraspinal locations.
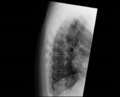
- Thoracic spine
There is flowing linear calcification and ossification along the anterior and right anterolateral vertebral bodies, continuing along the disc space, involving at least 4 contiguous vertebrae. There is a lucent area between the anterior longitudinal ligament and the mid-portion of the vertebral body. Right sided involvement is preponderant.
- Cervical spine
Hyperostosis is first seen along the anterior vertebral body, especially the inferior lip of the vertebra. A downward-pointing spur may be seen. The lower cervical spine is the most commonly affected. The hyperostosis is often symmetrical, and may cause displacement of the trachea and oesophagus. Ossifications are nonflowing on lateral imaging unlike the thoracic spine. Disc narrowing may be present. Ossification of the posterior longitudinal ligament (OPLL) is less common than ossification of the anterior longitudinal ligament.
- Lumbar spine
Radiographic findings are similar to the cervical spine. However the spurs tend to point upwards. Flowing ossification is less common than the thoracic spine. Complete bridging is uncommon. Disc narrowing may be present. OPLL is less common than in the cervical spine.
Rare findings are marginal sclerosis of the vertebral body, vacuum phenomena, and disc calcification. These findings are normally seen in degenerative disc disease but there may be overlap. OPLL is less common than in the cervical spine.
CT is more sensitive than plain x-ray at detecting OPLL. There may be two types of bridging patterns seen in OPLL One type seen in two thirds of patients is osteophyte fusion associated with a calcified anterior longitudinal ligament. The other type seen in the remaining patients is osteophyte fusion without apparent anterior longitudinal ligament calcification. These patterns appear occur concomitantly in patients.
Full-flowing osteophytosis appears to take 10 years to form.
Extraspinal involvement
Laboratory findings
Blood tests are usually normal or nondiagnostic. The following tests are normal or nondiagnostic: full blood count, ESR, calcium, phosphorus, growth hormone, liver function tests, parathyroid hormone, fluoride, protein eletrophoresis. HLA-B27 is not increased over the background rate.
Diagnosis
The diagnosis is made radiologically. It most commonly affects the thoracic spine. There may be suggestive symptoms, and signs such as spinal stiffness and reduced range of motion. Clinical features include: palpable bony spurs (e.g. at the calcaneus, patella, or olecranon); hyperostotic olecranon spurs (at the medial and lateral epicondyles with recurrent epicondylitis); soft tissue mass that is adherent to the quadriceips, patella, or Achilles tendon; generalised peripheral entheses tenderness; recurrent achilles tendinopathy; recurrent shoulder "bursitis"; dysphagia; myelopathy in those with ossification of the posterior longitudinal ligament; stridor.
The characteristic radiographic findings are flowing linear calcification and ossification along the anterior or right anterolateral aspects which continue along the disc spaces and involve at least four contiguous vertebrae. The disc height spaces should be largely preserved. Ankylosis is frequently incompletely. There can be interdigitating areas of protruding disc material in the flowing ossifications. There should be no sacroiliitis or facet joint ankylosis. There may be enthesopathy of the iliac crest, ischial tuberosities, and greater trochanters. Spur formation can occur in the appendicular skeleton including the olecranon, calcaneus, and patellar tendon. "Whiskering" enthesophytes may be seen.
A lateral thoracic spine x-ray is normally the first investigation. Try and view old chest x-ray films if available, as the changes may not be reported. When cervical spine, lumbar spine, or extra-spinal disease is suspected then obtain radiographic imaging of these areas. A chest radiograph will detect 75% of cases of DISH.
Differential Diagnosis
- Degenerative spine disease with osteophytosis otherwise known as spondylosis deformans. This is the most common condition that should be considered. The spurs may look similar but usually the anterior longitudinal ligament is not involved in degenerative disease.
- Ankylosing spondylitis. In this condition the bony bridges are normally slender and vertical ("bamboo spine"), so called syndesmophyte formation. They involve the outer margin of the annulus fibrosis without affecting the anterior longitudinal ligament. Vertical bone growth can also occur in DISH however, but horizontal growth (oseophytosis) is more common. Sacroiliac and apophyseal joint disease may occur but this is not seen in DISH. Sacroiliac involvement in AS involves the synovial inferior two-third portion of the joint, and occurs early on. Another differentiating feature seen in DISH but not ankylosing spondylitis, is bony excrescences adjacent to peripheral joints including the knee and elbow. On MRI bone marrow oedema and fat deposition may occur in both conditions.
- Ossification of the posterior longitudinal ligament. This may occur in up to 50% of patients with DISH, and is seen in the cervical spine. It can also occur independently or in association with spondyloarthropathies. It is more common in East Asian patients. Symptoms are often neurological in nature with myelopathy and radiculopathy, and surgery is often required in these instances. Asymptomatic patients can be monitored. Thoracic and lumbar OPLL can also occur.
- Acromegaly
- Hypoparathyroidism
- Fluorosis may cause paraspinal ligament calcification.
- Ochronosis
- Retinoid arthropathy causing skeletal hyperostosis, predominantly affecting the cervical spine.
- Trauma
- X-linked hypophosphatemic osteomalacia
Treatment
There are no randomised controlled trials on treatment modalities in DISH. Treatment may include reassurance, physical therapy, pharmacological therapy, and steroid injections.
Surgery may be required for anterior cervical osteophytes causing airway, cervical cord, or oesophageal symptoms. Ossification of the posterior longitudinal ligament may also require surgery if associated with myelopathic symptoms.
Patients with cervical spine involvement should be carefully counselled as to potential concerning symptoms that may indicate myelopathy, as well as symptoms of dysphagia and stridor. If undergoing airway or gastrointestinal procedures, patients with cervical spine disease may be at higher risk of complications.
Prognosis
The prognosis is generally good, however there is an increased rate of disability. In a large number of people it is an asymptomatic finding. Rarely potentially devastating complications can occur such as myelopathy and spinal fracture through ankylosed bone.