Interspinous Oedema: Difference between revisions
No edit summary |
No edit summary |
||
| Line 11: | Line 11: | ||
===Lumbar Kissing Spines=== | ===Lumbar Kissing Spines=== | ||
This condition, also known as Baastrup's disease, arises due to excessive lumbar lordosis, or following extension injuries to the lumbar spine. The adjacent spinous processes, the most common level being L4/5, compresses the intervening interspinous ligament. It is more common in the degenerative lumbar spine in those aged 70 and older, with no gender predilection, with changes occurring in the context of disc height loss, spondylolisthesis, and spondylosis.<ref name="Filippiadis"/><ref name="bogduk"/> | This condition, also known as Baastrup's disease, arises due to excessive lumbar lordosis, or following extension injuries to the lumbar spine. The adjacent spinous processes, the most common level being L4/5, compresses the intervening interspinous ligament. It is more common in the degenerative lumbar spine in those aged 70 and older, with no gender predilection, with changes occurring in the context of disc height loss, spondylolisthesis, and spondylosis.<ref name="Filippiadis"/><ref name="bogduk"/> | ||
==Epidemiology== | |||
There are no published data on the prevalence of symptomatic interspinous oedema. A New Zealand Musculoskeletal Medicine Physician conducted an audit of their practice over 12-18 months from December 2019. The term symptomatic was applied when there was interspinous oedema on MRI and significant improvement with a fluoroscopically guided injection. Of 178 new cases of low back pain +/- leg pain, there were 21 cases of symptomatic interspinous oedema (12% prevalence), 6 cases of asymptomatic interspinous oedema (3.3% prevalence), and 10 inconclusive cases (5.6% prevalence) | |||
==Clinical Features== | ==Clinical Features== | ||
The clinical experience of one Musculoskeletal Medicine Physician has found certain patterns in the presentation. The onset of pain is closely linked to the time of the accident/forces. The patient is definite about the accident. The pain distribution is highly variable. The pain is significant, and affects sleep, work, and recreation. On examination there is tenderness of the interspinous soft tissues. | |||
{| class="wikitable" | |||
|+ Case Examples of Symptomatic Interspinous Oedema | |||
|- | |||
! Age !! Duration of Pain !! Injury !! Interspace !! Pain Drawing | |||
|- | |||
| 39 || 8 months || Lifting rail 'ping' || L4/5 L5/S1 || [[File:ISO pain case 1.png|100px]] | |||
|- | |||
| 55 || 3 months || Fall|| L4/5|| [[File:ISO pain case 2.png|100px]] | |||
|- | |||
| 41 || 3 months|| Lifting at gym|| L4/5 L5/S1|| [[File:ISO pain case 3.png|100px]] | |||
|- | |||
| 30 || 1 month || Lifting child || L5/S1|| [[File:ISO pain case 4.png|100px]] | |||
|} | |||
In kissing spines, patients may have midline back pain that worsens with extension and relieved by flexion. On examination the patient may be tender over the suspected level. Rarely an epidural cystic mass may cause neurogenic claudication with extension.<ref name="Filippiadis"/> | |||
==Imaging== | ==Imaging== | ||
Revision as of 13:25, 26 June 2021
There are a variable number of bursae in the spinal column. They are normally located between the spinous processes of the cervical and lumbar segments. Bursitis of these structures can result in neck or back pain. In the neck, interspinous bursitis has been associated with several rheumatological conditions such as polymyalgia rheumatica, rheumatoid arthritis, and crystalopathies. In the lumbar spine the condition is also known as "kissing-spine" or Baastrup's disease and occurs in the context of degenerative change. An open access review of kissing spines is available by Filippiadis et al.[1]
Anatomy
There are several soft tissue structures located in the posterior aspect of the lumbar spines. Namely, the multifidi muscles, interspinalis muscles, interspinous ligaments, and fat. These structures are innervated by the medial branches of the lumbar dorsal rami, the same innervation as the facet joints.
Aetiology
Bogduk theorises that the pain arises as a result of a periostitis of the spinous processes, or inflammation of the interspinous ligament. The periosteum of the spinous processes and the interspinous spaces are innervated by the medial branches of the lumbar dorsal rami. [2]
Lumbar Kissing Spines
This condition, also known as Baastrup's disease, arises due to excessive lumbar lordosis, or following extension injuries to the lumbar spine. The adjacent spinous processes, the most common level being L4/5, compresses the intervening interspinous ligament. It is more common in the degenerative lumbar spine in those aged 70 and older, with no gender predilection, with changes occurring in the context of disc height loss, spondylolisthesis, and spondylosis.[1][2]
Epidemiology
There are no published data on the prevalence of symptomatic interspinous oedema. A New Zealand Musculoskeletal Medicine Physician conducted an audit of their practice over 12-18 months from December 2019. The term symptomatic was applied when there was interspinous oedema on MRI and significant improvement with a fluoroscopically guided injection. Of 178 new cases of low back pain +/- leg pain, there were 21 cases of symptomatic interspinous oedema (12% prevalence), 6 cases of asymptomatic interspinous oedema (3.3% prevalence), and 10 inconclusive cases (5.6% prevalence)
Clinical Features
The clinical experience of one Musculoskeletal Medicine Physician has found certain patterns in the presentation. The onset of pain is closely linked to the time of the accident/forces. The patient is definite about the accident. The pain distribution is highly variable. The pain is significant, and affects sleep, work, and recreation. On examination there is tenderness of the interspinous soft tissues.
In kissing spines, patients may have midline back pain that worsens with extension and relieved by flexion. On examination the patient may be tender over the suspected level. Rarely an epidural cystic mass may cause neurogenic claudication with extension.[1]
Imaging
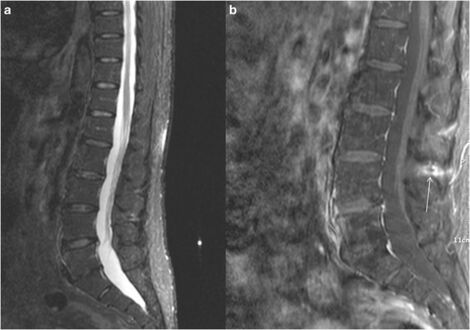
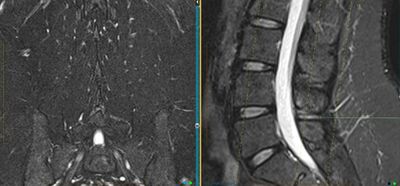
The diagnosis is supported by finding interspinous oedema on MRI. The two key sequences are the coronal fat sat Dixon and the T2 sagittal sequence. The coronal fat sat sequence needs to be specifically requested at certain radiology providers in New Zealand.
Kissing Spines
Imaging includes radiography, CT, and MRI. The hallmark finding suggestive of kissing spines is close approximation and contact of adjacent spinous processes with all the subsequent findings, including oedema, cystic lesions, sclerosis, flattening and enlargement of the articulating surfaces, bursitis and occasionally epidural cysts or midline epidural fibrotic masses.[1]
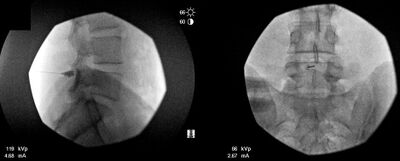
On x-rays, the most common finding is the close approximation and contact of adjacent spinous processes. There may be sclerosis of the articulating surfaces. In more severe cases, there is flattening and enlargement of the articulating surfaces or articulation of the two affected spinous processes. Usually generalised degenerative spinal changes are seen, most prominent at the affected level.[1]
CT shows close approximation and contact of the adjacent spinous processes. There is sclerosis, flattening, and enlargement of the articulating surfaces or the articulation of the two affected spinous processes. In rare cases there may be soft tissue nodules on the sides of the spinous process, and this could represent dissection of the spinal bursa superficial to the erector spinae. There are usually findings of degenerative changes such as facet joint hypertrophy, disc herniation, and spondylolisthesis.[1]
On MRI, under 10% of symptomatic patients have findings of interspinous bursitis. Bursitis appears as a fluid-like signal located between the two suspect spinous processes. Other findings include flattening, sclerosis, enlargement, cystic lesions, and bone oedema affecting the articulating surfaces of the two spinous processes. There may be oedema of the interspinous ligament. Gadolinium administration may show enhancement of this area. Rarely there may be epidural cysts or epidural fibrotic masses causing dural compression.[1]
MRI, STIR sequence, sagittal reconstruction illustrating bone oedema at both the spinous processes of L3-L4 level.[1]
Lumbar spine X-ray, AP (left image) and lateral (right image) views illustrating close approximation and contact of spinous processes at L4-L5 level with sclerosis and flattening of the articulating surfaces (white arrow).[1]
Diagnosis
There are no validated criteria for diagnosing symptomatic interspinous oedema. The diagnosis is supported by a consistent clinical picture, finding tenderness in the affected interspace, MRI findings of interspinous oedema on the appropriate sequences, and resolution of pain with infiltration of local anaesthetic under imaging guidance.
The interspinous soft tissues are supplied by the medial branch of the dorsal ramus. Therefore medial branch diagnostic blocks would be positive, and radiofrequency neurotomy of the medial branches would relieve the pain. There is discussion amongst the Musculoskeletal Medicine community as to whether, if the history fits, should symptomatic interspinous oedema be excluded by the appropriate MRI sequences before embarking on MBBs?
Treatment
Treatment options include NSAIDs, corticosteroid injections, and surgical therapies which include excision of the bursa or osteotomy. There may be additional factors in the patients pain such as facet joint irritation which may need to be addressed.
Injections
Injections are performed at the level of the interspinous ligament. This should ideally be done with imaging guidance to ensure accurate needle positioning. In New Zealand, fluoroscopic guidance is normally used, but ultrasound could theoretically be used as an alternative. There is usually durable fast relief by an interspinous injection of steroid and LA.
The technique used by one Musculoskeletal Physician in New Zealand is as follows:
- Advance a 9 cm 22-gauge spinal needle into the interspinous space using AP and lateral projections.
- Infiltrated 1 mL Omnipaque 300 into the interspinous space to ensure position.
- Infiltrate a mixture of 40 mg Kenacort A and 0.5 mL 0.75% Ropivacaine into the affected interspinous space.
Surgery
Surgical therapy is not always successful.
Summary
- The patient is definite about an accident with the pain being closely linked to the inciting event. The pain distribution is quite variable, but the pain intensity is often severe with marked effects on function. There is tenderness in the affected interspinous space.
- For diagnosis the MRI needs a coronal T2 fat sat Dixon sequence
- Durable fast relief by an interspinous injection of steroid and LA
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Filippiadis et al.. Baastrup's disease (kissing spines syndrome): a pictorial review. Insights into imaging 2015. 6:123-8. PMID: 25582088. DOI. Full Text.
- ↑ 2.0 2.1 Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Chapter 15. Edinburgh: Elsevier/Churchill Livingstone, 2012.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


![MRI, STIR sequence, sagittal reconstruction illustrating bone oedema at both the spinous processes of L3-L4 level.[1]](/w/img_auth.php/thumb/8/8d/Baastrup_kissing_spine_bone_oedema_MRI.jpg/331px-Baastrup_kissing_spine_bone_oedema_MRI.jpg)
![Lumbar spine X-ray, AP (left image) and lateral (right image) views illustrating close approximation and contact of spinous processes at L4-L5 level with sclerosis and flattening of the articulating surfaces (white arrow).[1]](/w/img_auth.php/thumb/f/f5/Baastrup_kissing_spine_XR.jpg/548px-Baastrup_kissing_spine_XR.jpg)