Neuronopathies
Neuronopathy means the cell body is affected rather than the myelin or axon as in peripheral neuropathy. This article is focused on the sensory neuronopathies where there is primary degeneration of the dorsal root ganglion and trigeminal ganglion sensory neurons.
Classification
The classification of neuropathic disorders is as follows
- Neuronopathies (pure sensory or pure motor or autonomic)
- Sensory neuronopathies (ganglionopathies)
- Motor neuronopathies (motor neuron disease)
- Autonomic neuropathies
- Peripheral neuropathies (usually sensorimotor)
- Myelinopathies
- Axonopathies
- Large- and small-fibre
- Small-fibre
Anatomy
The dorsal root ganglion (DRG) contains the cell bodies of sensory pseudo-unipolar neurons. The dorsal roots contain their efferent projections. Capillaries supply the DRG and in doing so cause fenestration and thereby loosening the blood-nerve barrier. This increases susceptibility to antibodies and toxins.
There are two populations of neurons in the DRG. These are the large-light cells with their Aβ and Aδ fibre projections. The other population, which are the majority of the cells, are the small-dark cells and their unmyelinated C fibres. The afferent projections of the larger neurons containing proprioceptive and tactile sensation traverse the posterior column.
Clinical Features
The sensory neuronopathies classically present with early onset sensory ataxia, potentially secondary to proximal muscle spindle and joint denervation.[1] Note, sensory ataxia can also be caused by large fibre neuropathy and pathology localised to the dorsal column.
If the small and medium sized nerves are also involved then the patient may experience neuropathic pain (positive sensory symptoms).
This leads to the other classic feature being that the negative symptoms (numbness) and positive symptoms often present with a non-length-dependent and multifocal pattern. This differentiates them from typical length dependent axonal sensory polyneuropathies. Misdiagnosis can occur if the examiner is testing sensation from distal to proximal and stops at the presumed sensory level, thereby missing the multifocal presentation.
Vestibular dysfunction can occur, such as in CANVAS syndrome .
Power is usually normal, but patients may appear weak due to lack of proprioceptive feedback.
The muscle stretch reflexes are often unelicitable.
Aetiology
- Immune mediated disease: Sjogren syndrome, systemic lupus erythematosus, autoimmune hepatitis, celiac disease
- Paraneoplastic disease: Small-cell lung cancer, bronchial carcinoma, breast cancer, ovarian cancer, Hodgkin lymphoma, transitional cell bladder cancer, prostate cancer, malignant mixed M€ullerian tumor, neuroendocrine tumor, sarcoma
- Viral infections: HIV, EBV, VZV, HTLV-1
- Vitamin B6
- Intoxication
- Neurotoxic drugs: pyridoxine, cisplatin, carboplatin, oxaliplatin
- Hereditary and degenerative disorders: hereditary sensory autonomic neuropathy (HSAN), Charcot-Marie-tooth disease type 2B (CMT2B), sensory ataxia neuropathy with dysarthria and ophthalmoparesis (SANDO), facial-onset sensory motor neuronopathy (FOSMN), and Cerebellar ataxia, neuropathy, vestibular areflexia syndrome (CANVAS)[1]
- Idiopathic
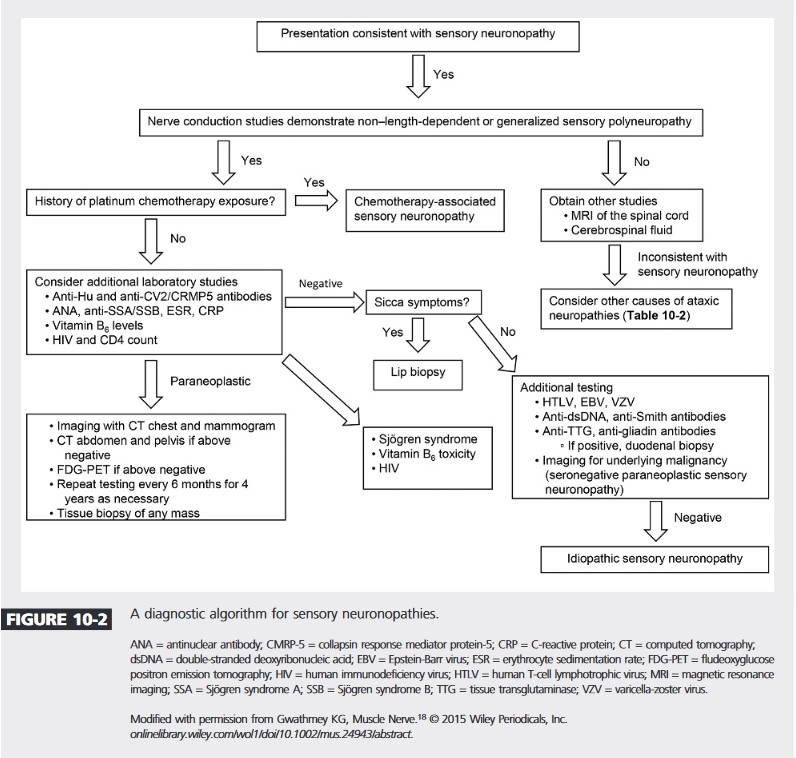
Investigations
References
- ↑ 1.0 1.1 Gwathmey, Kelly Graham (2016-01). "Sensory neuronopathies". Muscle & Nerve. 53 (1): 8–19. doi:10.1002/mus.24943. ISSN 1097-4598. PMID 26467754. Check date values in:
|date=(help) - ↑ Gwathmey, Kelly Graham (2017-10). "Sensory Polyneuropathies". CONTINUUM: Lifelong Learning in Neurology (in English). 23 (5): 1411–1436. doi:10.1212/CON.0000000000000518. ISSN 1538-6899. Check date values in:
|date=(help)

