Platelet Rich Plasma Injection
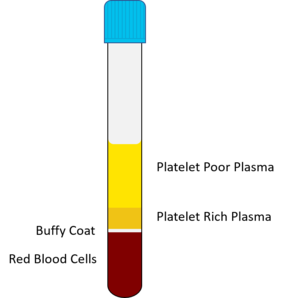
Platelet rich plasma (PRP) is an autologous blood product, with platelet levels at a higher level than baseline. The patient's blood is extracted, anticoagulated, spun down in a centrifuge, the PRP is extracted, and then injected. Platelets are involved in tissue repair through the release of growth factors. The centrifugation process can be done via a single-spin, or double-spin process for higher platelet concentrations, and is known as differential centrifugation. There is no consensus on activation, some authors prefer using an activator such as calcium chloride, while others argue against this.[1] The final platelet concentration, described in terms of times (e.g. 5x), varies between protocols, PRP cartridge kits, the age, and co-morbidities of the patient. However a higher platelet concentration is not necessarily more effective. The procedure can be repeated. [2]
Definitions
- Pure PRP (P-PRP): Has a low leucocyte content, and is injected as a liquid or gel. Prepared by extracting the upper layer and superficial buffy coat.
- Leucocyte-rich PRP (L-PRP): Higher platelet concentration than P-PRP, and can also be injected as an activated gel or liquid. Prepared by extracting the entire buffy coat and a few RBCs
- Pure platelet-rich fibrin (P-PRF): A platelet-rich fibrin scaffold, obtained by double-spinning centrifugation. This is stiffer than normal PRP and is in a gel form.
- Leucocyte- and platelet-rich fibrin (L-PRF): A non-injectable leucocyte-rich gel
Indications
Tendinopathy, mild osteoarthritis, cartilage tears etc
Contraindications
Blood disorders or platelet dysfunction. Haemoglobin level below 100, tumour in wound bed, metastatic disease, active infection. [2]
Risks
infection, bleed, nerve damage all rare
Pre-procedure Instructions
Stop NSAIDs and potentially anti-platelet prior to and just after (as long as not contraindicated to stop).
Procedure
Equipment
Procedure described for doing one leukocyte rich and one leukocyte poor injection. 30mL of blood will yield around 3-5mL of PRP depending on preparation, device, and patient factors.
- Syringes
- 60mL syringe for the blood
- 10mL syringe for the local anaesthetic
- 10mL syringe for the leukocyte poor PRP
- 10mL syringe for the leukocyte rich PRP
- Needles
- butterfly set for taking blood
- drawing up needle
- 25g needle for the local anaesthetic
- Needle for the PRP injection e.g. 22g 70mm spinal needle for the hip joint.
- ACDA anticoagulant
- PRP kit
- One cartridge for the blood
- Another cartridge as a counterbalance, measured to weigh the same, filled with water.
- Centrifuge
- Sterile ultrasound jelly
- Ultrasound machine
- PRP benchtop processing station.
Preparation
- Put ~2.5mL of ACDA into the 60mL syringe
- Draw up 55mL of blood into the 60mL syringe
- Place the drawing up needle onto the syringe, open the top of the cartridge, and then transfer the mixed blood/ACDA solution. Close the top
- Place the cartridge into the centrifuge, along with an equal counterweight cartridge.
- Spin as per per protocol. A single spin separates the whole blood into three layers. Namely, an upper layer containing mostly platelets and WBC, an intermediate buffy coat layer rich in WBCs, and a bottom layer containing mostly RBCs.[1]
- One spin at 1500rpm for 5 minutes: producing a low platelet and low WBC solution
- One spin at 3200rpm for 15 minutes: producing a high platelet and high WBC solution
- Double spin process: producing a high platelet solution
- First spin 1500rpm for 5 minutes,
- For pure PRP, after the first spin transfer the upper layer and superficial buffy coat into an empty tube. For leucocyte rich PRP transfer the upper layer, entire buffy coat, and a few RBCs.
- Second spin 6300rpm for 20 minutes. The lower one third is platelet rich plasma (PRP), the upper two thirds is platelet poor plasma (PPP).
- Place the tube into the PRP benchtop processing station
- Use the dial on the station to control the plunger
- Remove and discard the platelet poor plasma (upper two thirds).
- For two spin protocols, platelet pellets are seen at the bottom of the tube. Homogenise the pellets by thoroughly mixing.
- Transfer the top remaining half (leukocyte poor PRP) into a 10mL syringe
- Transfer the bottom remaining half, including some of the leukocytes (leukocyte rich PRP) into another 10mL syringe.
Procedure
- Joint
- Infiltrate the skin and capsule with local anaesthetic but not the joint space
- Inject into the joint space or joint structure with the leukocyte poor solution
- Tendon
- Inject around the tendon with the leukocyte rich solution
Aftercare
- Leukocyte rich PRP can cause a pain flare for a few days.
- Advise to wait for minimum 4 weeks before assessing efficacy.
- Use joint gently after procedure (e.g. low resistance cycling).
- 3 x injections for maximal effect
- Stop NSAIDs and potentially anti-platelet prior to and just after (as long as not contraindicated to stop).
Resources
{{#l:Platelet-rich plasma (PRP) for knee disorders.pdf}}
References
- ↑ 1.0 1.1 Dhurat & Sukesh. Principles and Methods of Preparation of Platelet-Rich Plasma: A Review and Author's Perspective. Journal of cutaneous and aesthetic surgery 2014. 7:189-97. PMID: 25722595. DOI. Full Text.
- ↑ 2.0 2.1 Shahid & Kundra. Platelet-rich plasma (PRP) for knee disorders. EFORT open reviews 2017. 2:28-34. PMID: 28607768. DOI. Full Text.