Sacral Insufficiency Fracture: Difference between revisions
| Line 33: | Line 33: | ||
=== Plan Films === | === Plan Films === | ||
Plain films are not very sensitive at picking up sacral insufficiency fractures, with them only being detected in 20-38% of cases.. Part of this is because dedicated sacral views are often not taken. When visible there is a vertical sclerotic band in zone 1 in 57% of cases, with a fracture line in 12% of cases. | Plain films are not very sensitive at picking up sacral insufficiency fractures, with them only being detected in 20-38% of cases.. Part of this is because dedicated sacral views are often not taken. When visible there is a vertical sclerotic band in zone 1 in 57% of cases, with a fracture line in 12% of cases.<ref name=":0" /> | ||
=== High Tech Imaging === | === High Tech Imaging === | ||
MRI has a sensitivity of close to 100%. It is very important that coronal oblique views of the sacrum are included. The fracture may be missed if "lumbar spine MRI" is requested. In New Zealand lumbar spine MRI and pelvis MRI are two separate scans for funding and insurance purposes. | MRI has a sensitivity of close to 100%. It is very important that coronal oblique views of the sacrum are included. The fracture may be missed if "lumbar spine MRI" is requested. In New Zealand lumbar spine MRI and pelvis MRI are two separate scans for funding and insurance purposes.<ref name=":0" /> | ||
CT has a sensitivity of 60-75%, however it can be helpful for surgical planning as well as differentiating between metastatic disease and fracture. | CT has a sensitivity of 60-75%, however it can be helpful for surgical planning as well as differentiating between metastatic disease and fracture.<ref name=":0" /> | ||
=== DEXA === | === DEXA === | ||
Almost all patients will have severe osteopenia on DEXA imaging. | Almost all patients will have severe osteopenia on DEXA imaging. | ||
== | == Management == | ||
The optimal treatment approach is unknown. Most patients improve with conservative care. It varies between 6 to 15 months for recovery. However 50% do not return to their premorbid state, and mortality is 14.3%.<ref name=":0" /> | |||
Prolonged bedrest may be recommended but this carries the potential for increased morbidity. For example it is important to be alert to venous thromboembolism. DVTs occur in 29-61% of cases, and PE in 2-12%. | |||
== References == | == References == | ||
[[Category:Fractures]] | [[Category:Fractures]] | ||
[[Category:Pelvis, Hip and Thigh Conditions]] | [[Category:Pelvis, Hip and Thigh Conditions]] | ||
Revision as of 19:17, 15 November 2022
Epidemiology
This condition classical affects osteoporotic elderly women. The mean age is 70-75, with almost all patients older than 55.[1]
Other risk factors include prior pelvic radiation (prevalence 21-89%), prolonged glucocorticoid use, rheumatoid arthritis, multiple myeloma, Paget disease, renal osteodystrophy, and hyperparathyroidism. [1]
Anatomy
- Main article: Sacrum
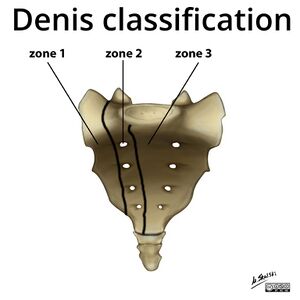
The sacrum is a triangular bone and when talking about insufficiency fractures it is viewed as having three zones:
- Zone 1: The sacral ala lateral to the foraminae
- Zone 2: the area involving the neural foraminae
- Zone 3: medial the the neural foraminae, containing the sacral bodies.
Pathology
Insufficiency fractures are a subtype of stress fracture where normal stress is applied to bone with reduced elastic resistance. This is usually due to osteoporosis. Other causes of insufficiency fractures are metastatic disease and bone marrow infiltration processes.
They most commonly affect the sacral ala, in a sagittal line lateral to the sacral foraminae and medial to the sacral iliac joints, called zone 1. There is an equal prevalence of unilateral versus bilateral fractures. In some cases there is a fracture line component in the axial plane.
The reason that the sacral ala are affected is because in osteoporosis there isn't uniform bone loss. There is relatively increased loss of bony trabeculae in the sacral alae compared to the vertebra bodies.
There is a high prevalence of concomitant fractures of the pubic rami and parasymphyseal region. There can also be additional fractures in the superior acetabulum and iliac wing. It is thought that the sacral ala fractures happen first which then results in a cascade of abnormal biomechanics resulting in fractures elsewhere.
Clinical Features
History
In two thirds of patients there is no trauma, and when there is trauma it is usually minor. Patients will commonly have diffuse low back pain with radiation to the buttock, hip, or groin. 45% of patients have a history of malignancy.[1]
Examination
There may be lumbosacral spine tenderness. There is usually no neurological deficit, however rarely patients can manifest with a sacral radiculopathy or even cauda equina syndrome.
Investigations
Plan Films
Plain films are not very sensitive at picking up sacral insufficiency fractures, with them only being detected in 20-38% of cases.. Part of this is because dedicated sacral views are often not taken. When visible there is a vertical sclerotic band in zone 1 in 57% of cases, with a fracture line in 12% of cases.[1]
High Tech Imaging
MRI has a sensitivity of close to 100%. It is very important that coronal oblique views of the sacrum are included. The fracture may be missed if "lumbar spine MRI" is requested. In New Zealand lumbar spine MRI and pelvis MRI are two separate scans for funding and insurance purposes.[1]
CT has a sensitivity of 60-75%, however it can be helpful for surgical planning as well as differentiating between metastatic disease and fracture.[1]
DEXA
Almost all patients will have severe osteopenia on DEXA imaging.
Management
The optimal treatment approach is unknown. Most patients improve with conservative care. It varies between 6 to 15 months for recovery. However 50% do not return to their premorbid state, and mortality is 14.3%.[1]
Prolonged bedrest may be recommended but this carries the potential for increased morbidity. For example it is important to be alert to venous thromboembolism. DVTs occur in 29-61% of cases, and PE in 2-12%.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Lyders, E. M.; Whitlow, C. T.; Baker, M. D.; Morris, P. P. (2010-02). "Imaging and treatment of sacral insufficiency fractures". AJNR. American journal of neuroradiology. 31 (2): 201–210. doi:10.3174/ajnr.A1666. ISSN 1936-959X. PMC 7964142. PMID 19762463. Check date values in:
|date=(help)