Slipping Rib Syndrome: Difference between revisions
m (Jeremy moved page Slipped Rib Syndrome to Slipping Rib Syndrome) |
No edit summary |
||
| Line 1: | Line 1: | ||
{{ | {{partial}} | ||
Slipped rib syndrome is a poorly understood, but potentially under-recognised cause for chronic chest wall pain. | {{condition | ||
|image= | |||
|name= | |||
|taxonomy= | |||
|synonym= | |||
|definition= | |||
|epidemiology=Any age, females > males | |||
|causes= | |||
|pathophysiology= loss of fibrous or cartilaginous attachments between ribs 8-10 causing subluxation and intercostal nerve impingement. | |||
|classification= | |||
|primaryprevention= | |||
|secondaryprevention= | |||
|riskfactors=hypermobility | |||
|clinicalfeatures= | |||
|history=Lower rib cage pain | |||
|examination=Palpable separation of ≥1cm at insertion of any 8-10th rib cartilages, rib hypermobility, separation point tenderness. | |||
|diagnosis=Can usually be diagnosed on history and exam | |||
|tests=Dynamic ultrasound | |||
|ddx= | |||
|treatment=Nerve blocks, manipulation, topical analgesia, rib excision, Hansen repair | |||
|prognosis= | |||
}} | |||
Slipped rib syndrome is a poorly understood, but potentially under-recognised cause for chronic chest wall pain. The pain arises a lower anterior rib subluxes and causes pain due to impingement of the intercostal nerves. | |||
==Anatomy== | ==Anatomy== | ||
The | The true ribs are ribs 1-7 and have direct cartilaginous attachments to the sternum. | ||
Ribs 8-10 are the false ribs are joined together anteriorly through a cartilaginous cap or fibrous band, called the interchondral joints. The interchondral joints normally merge into a common arch joining to the sternum. The false ribs "piggyback" on the 7th true rib cartilage. The interchondral joints provide some stability and flexibility with movement and breathing. The diaphragm connects to the false ribs, using them as an anchor point for activation.<ref name="youtube-hansen"/> | |||
Ribs 11-12 are floating and do not have an attachment to the other cartilages or sternum. | |||
==Epidemiology== | ==Epidemiology== | ||
The diagnosis has been documented in 1% of all general medical referrals, and 5% of new gastroenterology referrals.<ref name="youtube-hansen"/> In research by Hansen et al, the mean age was 51, 90% were female, 38% have a history of trauma, the average duration of pain was 38 months. The patients tended to be at the end of the line with 41% had suicidal ideations due to pain severity.<ref name="Hansen"/> | The diagnosis has been documented in 1% of all general medical referrals, and 5% of new gastroenterology referrals.<ref name="youtube-hansen"/> In research by Hansen et al, the mean age was 51 (it can occur in any age group), 90% were female, 38% have a history of trauma, the average duration of pain was 38 months. The patients tended to be at the end of the line with 41% had suicidal ideations due to pain severity.<ref name="Hansen"/> <ref name="mcmahon"/> | ||
== | ==Aetiopathophysiology== | ||
[[File:slipped rib anatomy.png|thumb|right|Slipped rib syndrome anatomy<ref name="youtube-hansen"/>]] | [[File:slipped rib anatomy.png|thumb|right|Slipped rib syndrome anatomy<ref name="youtube-hansen"/>]] | ||
The condition occurs when the costal cartilages of the false ribs (8-10) lose their fibrous or cartilaginous attachments to each other. One of the ribs is then able to sublux either anteriorly or posteriorly with movement sliding beneath an adjacent rib. This causes irritation of the intercostal nerves. The cartilagenous tips or fibrous attachments must be disrupted in order for these ribs to move.<ref name="mcmahon"/> | |||
Damage to the cartilage can occur due to trauma, degenerative change, and hypermobile connective tissue disorders. The condition is a joint dislocation. It most commonly involves the 10th rib, but can involve additional ribs. In Dr Adam Hansen's experience, the 10th rib is always involved.<ref name="youtube-hansen">https://www.youtube.com/watch?v=EZDFe3fC6ck</ref> Typically the affected rib will slip towards and under the rib above, impinging the intercostal nerve between the two. This can occur with simple every day movements, and can cause chronic pain. | |||
==Clinical Manifestations== | ==Clinical Manifestations== | ||
The pain is dermatomal, and typically extends to the back over the costovertebral joint. It can also refer to the upper abdomen. It can be confused with visceral pathology.<ref name="youtube-hansen"/> | ===History=== | ||
The pain is intermittent, usually severe, and is usually over the lower rib cage. The initial pain is sharp and stabbing that lasts a few minutes, with a secondary aching or burning pain that lasts several hours.{{#pmid:30078490|mcmahon}} The pain is dermatomal, and typically extends to the back over the costovertebral joint. It can also refer to the upper abdomen. It can be confused with visceral pathology.<ref name="youtube-hansen"/> It can cause nausea or vomiting when severe which can further confuse matters.<ref name="mcmahon"/> | |||
It often occurs with movement such as twisting, bending, deep breathing, sitting, sneezing, or coughing. There may be a popping or grinding sensation and they may be able to demonstrate the rib subluxing.<ref name="mcmahon"/> | |||
There may or may not be a history of trauma - sudden extension or flexion, vigorous swimming, or repeated one-sided exercise such as one-sided weight bearing, ball throwing, or bat swinging.<ref name="mcmahon"/> | |||
Some patients have temporary relief with stretching of the affected side or putting pressure over the area. Patients often report needing to rest for prolonged periods until the pain eases. Bilateral symptoms can occur but usually there is one dominant side.<ref name="mcmahon"/> | |||
A common theme in case reports is significant delay to diagnosis and misdiagnosis, and even incorrectly labelling of the patient's pain being psychosomatic.<ref name="mcmahon"/> | |||
===Physical examination=== | ===Physical examination=== | ||
Dr Hansen uses the following criteria for diagnosis on physical examination<ref name="youtube-hansen"/> | Dr Hansen uses the following criteria for diagnosis on physical examination<ref name="youtube-hansen"/> | ||
| Line 22: | Line 59: | ||
*Palpation at the separation point reproduces the patient's pain | *Palpation at the separation point reproduces the patient's pain | ||
The above is less painful than the traditional hook manoeuvre which is where the examiner slides their fingers under the costal margin lifting it anteriorly and superiorly looking for movement and pain. | |||
==Imaging== | |||
The condition can be assessed via dynamic ultrasound.<ref>{{#pmid:11883545}}</ref><ref>{{#pmid:30612161}}</ref> This involves visualising the cartilage with certain movements looking for the ribs moving under or abutting each other during. Visualisation during a crunch manoeuvre and pushing along the cartilages may be sufficient for diagnosis with a sensitivity of 92% and specificity of 100% in one study.<ref name="mcmahon"/> | |||
This type of imaging assessment does not seem to be taught to MSK Sonographers in New Zealand at the time of writing, and so the study quality is likely to be variable. | |||
==Diagnosis== | |||
History and examination findings are often sufficient for diagnosis. A local anaesthetic intercostal nerve block can be used to define the level of nerve irritation.<ref name="mcmahon"/> | |||
==Differential Diagnosis== | |||
{{DDX Box | |||
|ddx-text= | |||
*Somatic referred or radicular pain from the thoracic spine | |||
*Abdominal wall strain or abdominal cutaneous nerve entrapment | |||
*Intercostal neuritis | |||
*Hepatobiliary or splenic disease | |||
*Dyspepsia or oesophagitis | |||
*Pancreatitis | |||
*Renal colic | |||
*Rib fracture | |||
*Costochondritis | |||
*Lung pathology | |||
}} | |||
==Treatment== | ==Treatment== | ||
Nonsurgical therapies have been reported by many authors to be ineffective.<ref name="youtube-hansen"/> | Reassurance may be all the is required for some patients. | ||
Nonsurgical therapies have been reported by many authors to be ineffective.<ref name="youtube-hansen"/> There have been reports of long lasting results with repeated nerve blocks, manipulative techniques, acupuncture, and topical analgesics.<ref name="mcmahon"/> | |||
===Injections=== | ===Injections=== | ||
Intercostal nerve blocks | Intercostal nerve blocks can provide symptom relief, but the rebound pain can be severe in some cases. It is recommended to block the entire nerve as well as the two adjacent nerves. This is a reasonable starting point if conservative management has failed. | ||
===Ablation=== | ===Ablation=== | ||
===Surgical=== | ===Surgical=== | ||
Rib excision is the traditional technique. | |||
A new less invasive technique known as Hansen repair has been described{{#pmid:32330472|Hansen}} See a video of the technique [https://www.youtube.com/watch?v=o8qJMU-TEmE here], and a webinar by Dr Hansen [https://www.youtube.com/watch?v=EZDFe3fC6ck here]. | |||
==Videos== | ==Videos== | ||
Revision as of 18:35, 5 June 2021
| Slipping Rib Syndrome | |
|---|---|
| Epidemiology | Any age, females > males |
| Pathophysiology | loss of fibrous or cartilaginous attachments between ribs 8-10 causing subluxation and intercostal nerve impingement. |
| Risk Factors | hypermobility |
| History | Lower rib cage pain |
| Examination | Palpable separation of ≥1cm at insertion of any 8-10th rib cartilages, rib hypermobility, separation point tenderness. |
| Diagnosis | Can usually be diagnosed on history and exam |
| Tests | Dynamic ultrasound |
| Treatment | Nerve blocks, manipulation, topical analgesia, rib excision, Hansen repair |
Slipped rib syndrome is a poorly understood, but potentially under-recognised cause for chronic chest wall pain. The pain arises a lower anterior rib subluxes and causes pain due to impingement of the intercostal nerves.
Anatomy
The true ribs are ribs 1-7 and have direct cartilaginous attachments to the sternum.
Ribs 8-10 are the false ribs are joined together anteriorly through a cartilaginous cap or fibrous band, called the interchondral joints. The interchondral joints normally merge into a common arch joining to the sternum. The false ribs "piggyback" on the 7th true rib cartilage. The interchondral joints provide some stability and flexibility with movement and breathing. The diaphragm connects to the false ribs, using them as an anchor point for activation.[1]
Ribs 11-12 are floating and do not have an attachment to the other cartilages or sternum.
Epidemiology
The diagnosis has been documented in 1% of all general medical referrals, and 5% of new gastroenterology referrals.[1] In research by Hansen et al, the mean age was 51 (it can occur in any age group), 90% were female, 38% have a history of trauma, the average duration of pain was 38 months. The patients tended to be at the end of the line with 41% had suicidal ideations due to pain severity.[2] [3]
Aetiopathophysiology
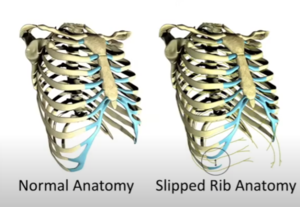
The condition occurs when the costal cartilages of the false ribs (8-10) lose their fibrous or cartilaginous attachments to each other. One of the ribs is then able to sublux either anteriorly or posteriorly with movement sliding beneath an adjacent rib. This causes irritation of the intercostal nerves. The cartilagenous tips or fibrous attachments must be disrupted in order for these ribs to move.[3]
Damage to the cartilage can occur due to trauma, degenerative change, and hypermobile connective tissue disorders. The condition is a joint dislocation. It most commonly involves the 10th rib, but can involve additional ribs. In Dr Adam Hansen's experience, the 10th rib is always involved.[1] Typically the affected rib will slip towards and under the rib above, impinging the intercostal nerve between the two. This can occur with simple every day movements, and can cause chronic pain.
Clinical Manifestations
History
The pain is intermittent, usually severe, and is usually over the lower rib cage. The initial pain is sharp and stabbing that lasts a few minutes, with a secondary aching or burning pain that lasts several hours.[3] The pain is dermatomal, and typically extends to the back over the costovertebral joint. It can also refer to the upper abdomen. It can be confused with visceral pathology.[1] It can cause nausea or vomiting when severe which can further confuse matters.[3]
It often occurs with movement such as twisting, bending, deep breathing, sitting, sneezing, or coughing. There may be a popping or grinding sensation and they may be able to demonstrate the rib subluxing.[3]
There may or may not be a history of trauma - sudden extension or flexion, vigorous swimming, or repeated one-sided exercise such as one-sided weight bearing, ball throwing, or bat swinging.[3]
Some patients have temporary relief with stretching of the affected side or putting pressure over the area. Patients often report needing to rest for prolonged periods until the pain eases. Bilateral symptoms can occur but usually there is one dominant side.[3]
A common theme in case reports is significant delay to diagnosis and misdiagnosis, and even incorrectly labelling of the patient's pain being psychosomatic.[3]
Physical examination
Dr Hansen uses the following criteria for diagnosis on physical examination[1]
- Palpable separation of ≥1cm at insertion of any 8-10th rib onto the costal arch
- Same rib hypermobile on palpation
- Palpation at the separation point reproduces the patient's pain
The above is less painful than the traditional hook manoeuvre which is where the examiner slides their fingers under the costal margin lifting it anteriorly and superiorly looking for movement and pain.
Imaging
The condition can be assessed via dynamic ultrasound.[4][5] This involves visualising the cartilage with certain movements looking for the ribs moving under or abutting each other during. Visualisation during a crunch manoeuvre and pushing along the cartilages may be sufficient for diagnosis with a sensitivity of 92% and specificity of 100% in one study.[3]
This type of imaging assessment does not seem to be taught to MSK Sonographers in New Zealand at the time of writing, and so the study quality is likely to be variable.
Diagnosis
History and examination findings are often sufficient for diagnosis. A local anaesthetic intercostal nerve block can be used to define the level of nerve irritation.[3]
Differential Diagnosis
- Somatic referred or radicular pain from the thoracic spine
- Abdominal wall strain or abdominal cutaneous nerve entrapment
- Intercostal neuritis
- Hepatobiliary or splenic disease
- Dyspepsia or oesophagitis
- Pancreatitis
- Renal colic
- Rib fracture
- Costochondritis
- Lung pathology
Treatment
Reassurance may be all the is required for some patients.
Nonsurgical therapies have been reported by many authors to be ineffective.[1] There have been reports of long lasting results with repeated nerve blocks, manipulative techniques, acupuncture, and topical analgesics.[3]
Injections
Intercostal nerve blocks can provide symptom relief, but the rebound pain can be severe in some cases. It is recommended to block the entire nerve as well as the two adjacent nerves. This is a reasonable starting point if conservative management has failed.
Ablation
Surgical
Rib excision is the traditional technique.
A new less invasive technique known as Hansen repair has been described[2] See a video of the technique here, and a webinar by Dr Hansen here.
Videos
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 https://www.youtube.com/watch?v=EZDFe3fC6ck
- ↑ 2.0 2.1 Hansen et al.. Minimally Invasive Repair of Adult Slipped Rib Syndrome Without Costal Cartilage Excision. The Annals of thoracic surgery 2020. 110:1030-1035. PMID: 32330472. DOI.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 McMahon. Slipping Rib Syndrome: A review of evaluation, diagnosis and treatment. Seminars in pediatric surgery 2018. 27:183-188. PMID: 30078490. DOI.
- ↑ Meuwly et al.. Slipping rib syndrome: a place for sonography in the diagnosis of a frequently overlooked cause of abdominal or low thoracic pain. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine 2002. 21:339-43. PMID: 11883545. DOI.
- ↑ Van Tassel et al.. Dynamic ultrasound in the evaluation of patients with suspected slipping rib syndrome. Skeletal radiology 2019. 48:741-751. PMID: 30612161. DOI.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


