Trigeminal Neuralgia
| |
| Trigeminal Neuralgia | |
|---|---|
| Classification | Classical, secondary, idiopathic. |
| Clinical Features | Recurrent episodes of unilateral facial pain confined to the trigeminal distribution |
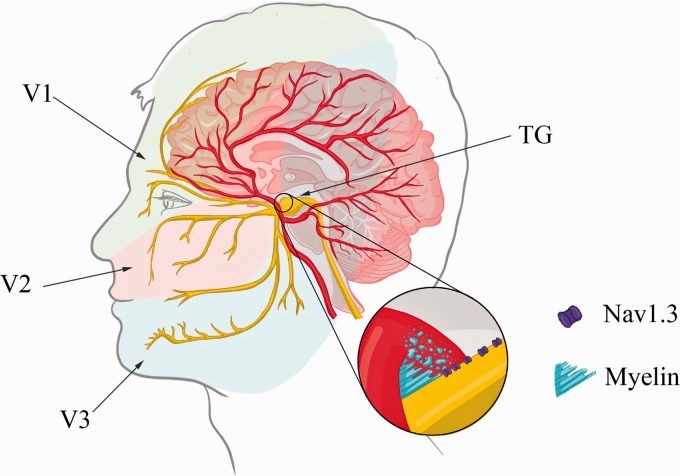
Trigeminal Neuralgia (TN) is a highly debilitating condition marked by intense, short-lived, and electric shock-like episodes of facial pain that occur repeatedly.
Investigations
MRI should be incorporated into the diagnostic evaluation of TN to assess for the primary form of the disease.
Clinical Features
Trigeminal Neuralgia is characterized by recurrent episodes of unilateral facial pain confined to the trigeminal distribution. These painful paroxysms last anywhere from a fraction of a second up to 2 minutes and are marked by severe electric shock-like, shooting, stabbing, or sharp sensations. Innocuous stimuli often precipitate these episodes.
Diagnosis
| International Classification of Headache Disorders edition 3 (ICHD-3) diagnostic criteria for trigeminal neuralgia |
|---|
| A. Recurrent paroxysms of unilateral facial pain in the distribution(s) of one or more divisions of the trigeminal nerve, with no radiation beyond, and fulfilling criteria B and C.
B. Pain has all of the following characteristics:
C. Precipitated by innocuous stimuli within the affected trigeminal distribution. D. Not better accounted for by another ICHD-3 diagnosis |
Classification
TN is divided into classical, secondary, or idiopathic subtypes based on the underlying cause. Classical TN, the most common subtype accounting for 75% of cases, is diagnosed when trigeminal neurovascular compression with morphological changes is present ipsilateral to the side of the pain. This can be demonstrated through MR imaging with appropriate trigeminal sequences or during surgery. Simple trigeminal contact without morphological changes does not warrant this diagnosis, as it is a common neuroimaging finding in healthy individuals. Prospective trigeminal MR imaging studies have revealed that classical TN is linked to neurovascular compression with morphological changes (distortion, indentation, atrophy) on the symptomatic side, while such changes are rare on the asymptomatic side.
Secondary TN, which accounts for approximately 15% of cases, is caused by an identifiable neurological disorder (excluding trigeminal neurovascular compression) known to trigger TN, such as cerebellopontine angle tumors, arteriovenous malformations, and multiple sclerosis. Roughly 2% of people with multiple sclerosis experience symptoms resembling TN.
Idiopathic TN, constituting about 10% of cases, is diagnosed when no apparent cause for the condition can be identified. Both idiopathic and classical TN are further divided into groups with purely paroxysmal pain or with concomitant continuous pain, based on the presence or absence of continuous or near-continuous interictal pain.
Management
Carbamazepine![]() and oxcarbazepine are considered first-line medications for TN. Additional treatment options include lamotrigine, gabapentin, pregabalin, botulinum toxin type A, and baclofen. These drugs can be used either as standalone treatments or in conjunction with other therapies.
and oxcarbazepine are considered first-line medications for TN. Additional treatment options include lamotrigine, gabapentin, pregabalin, botulinum toxin type A, and baclofen. These drugs can be used either as standalone treatments or in conjunction with other therapies.
In cases where pain is inadequately managed or patients experience poor tolerance to medical treatments, surgery may be considered. Trigeminal microvascular decompression is the preferred surgical approach for patients with trigeminal neurovascular conflict. Alternatively, neuroablative surgical procedures may be offered in instances where MR imaging does not reveal neurovascular contact or when patients are deemed too frail for microvascular decompression, or if they are unwilling to assume the associated risks.
Resources
References
- ↑ Gambeta E, Chichorro JG, Zamponi GW. Trigeminal neuralgia: An overview from pathophysiology to pharmacological treatments. Mol Pain. 2020 Jan-Dec;16:1744806920901890. doi: 10.1177/1744806920901890. PMID: 31908187; PMCID: PMC6985973.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


