Vertigo and Dizziness: Difference between revisions
No edit summary |
No edit summary |
||
| Line 20: | Line 20: | ||
[[File:Vestibulospinal tract.png|600px]] | [[File:Vestibulospinal tract.png|600px]] | ||
There are multiple sources of indirect evidence for abnormal sensory inputs in cervical dizziness. | |||
*Noxious stimulation of posterior neck muscles (such as vibration) can cause dizziness | |||
*Local anaesthetic injections to upper cervical nerves or muscles can cause dizziness. | |||
*Whiplash leads to deficits in neck position sense. | |||
*There may be relief of vertigo with a medial branch block in whiplash.<ref>{{#pmid:29871373}}</ref> | |||
*Manual therapy seems to be effective.{{#pmid:26218949|reid}} | |||
*There is often a disturbance in vestibulospinal control of optokinetic pursuit: Eye pursuit normal with static head, abnormal with head rotation. | |||
Cervical vertigo may result from a sensory mismatch between vestibular and cervical inputs, with altered input form the upper cervical proprioceptors to the vestibular nuclei.<ref name="Li"/> In whiplash cervical input may be dominant over vestibular with neck activation when there is pain or stiffness.<ref>Magnusen 2006</ref> The neural mismatch model describes a mismatch between centrally expected and actual neck movement From neck pain/stiffness, inducing motion sickness. <ref>{{#pmid:26826207}}</ref> | |||
The neural mismatch model describes a mismatch between expected and actual neck movement From neck pain/stiffness, inducing motion sickness. <ref>{{#pmid:26826207}}</ref> | |||
===Migraine Associated Cervicogenic Vertigo=== | ===Migraine Associated Cervicogenic Vertigo=== | ||
Revision as of 10:24, 1 November 2020
Cervical Vertigo
Cervical Vertigo, also known as cervicogenic vertigo or cervicogenic dizziness is a controversial entity. There is evidence that it is a distinct disorder but there is no agreed upon pathophysiology, reliable test, or diagnostic criteria. Reliable and well established tests support an alternative diagnosis in almost all patients with vertigo. [1] In centres with advanced capabilities for assessing vertigo, cervical vertigo is rare. However in settings of neck trauma, dizziness is common.
All clinical studies on the condition have three major weak points: inability to confirm the diagnosis, no specific laboratory test, and unexplained discrepancy between those with severe neck pain with no vertigo and those with moderate neck pain with severe vertigo.[1]
There are multiple models that attempt to explain cervical dizziness, and they are discussed in the sections below.
Abnormal Sensory Input
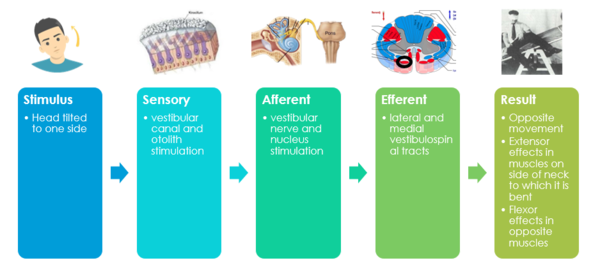
The Vestibulospinal reflex is a system for maintaining balance, posture, and, stability. When you close your eyes, the to and fro swaying is the vestibulospinal system righting the body. Some authors further subdivide the terminology and say that the vestibulospinal reflex is for muscles below the neck, and the vestibulochollic reflex if for the neck muscles. There is no objective test for detecting deficient or excessive vestibulospinal activity.
Cervical facet joints densely innervated, 50% of all cervical proprioceptors in joint capsules C1-C3. There are dense mechanoreceptors in the gamma-muscle spindles of deep segmental upper cervical muscles. Mechanoreceptor function can be altered by pain, trauma, fatigue, degeneration. There are direct connections to the vestibular and visual systems.[1]
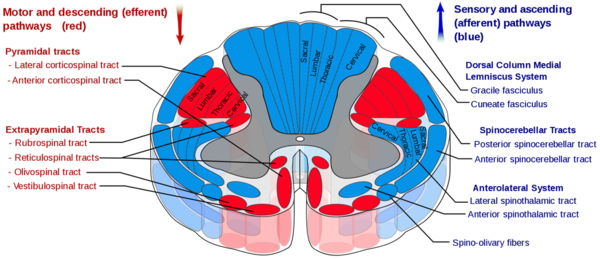
The vestibulospinal tract is a descending motor pathway (extrapyramidal) that gives motor commands that control posture. The medial tract is for neck muscles, head stabilisation / coordination, and eye movement. The lateral tract is for antigravity muscles, the leg extensors for upright posture.
There are multiple sources of indirect evidence for abnormal sensory inputs in cervical dizziness.
- Noxious stimulation of posterior neck muscles (such as vibration) can cause dizziness
- Local anaesthetic injections to upper cervical nerves or muscles can cause dizziness.
- Whiplash leads to deficits in neck position sense.
- There may be relief of vertigo with a medial branch block in whiplash.[2]
- Manual therapy seems to be effective.[3]
- There is often a disturbance in vestibulospinal control of optokinetic pursuit: Eye pursuit normal with static head, abnormal with head rotation.
Cervical vertigo may result from a sensory mismatch between vestibular and cervical inputs, with altered input form the upper cervical proprioceptors to the vestibular nuclei.[1] In whiplash cervical input may be dominant over vestibular with neck activation when there is pain or stiffness.[4] The neural mismatch model describes a mismatch between centrally expected and actual neck movement From neck pain/stiffness, inducing motion sickness. [5]
Migraine Associated Cervicogenic Vertigo
Vestibular migraine is the second most common cause of vertigo after BPPV. Migraine could be a link between cervical pain and vertigo through connections between the vestibular and trigeminal nuclei.[1]
Assessment
History
- Pain in back of neck, radiates temporo-parietally, may only be present with palpation
- Symptoms worse with neck pain and neck movement
- Symptoms better with interventions that relieve neck pain
- Vertigo lasts minutes to hours
- History of neck injury
Examination
- Reproducible vertigo with neck manipulation
- Tender suboccipitally, C1 and C2 transverse processes
- Tender C2 and C3 spinous processes
- Tender myofascial structures
- Upper C-spine range of motion
- No definitive diagnostic test
Treatment
Both Mulligan (in the form of cervical SNAGs) and Maitland mobilisations appear to be beneficial.[3]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Li & Peng. Pathogenesis, Diagnosis, and Treatment of Cervical Vertigo. Pain physician 2015. 18:E583-95. PMID: 26218949.
- ↑ Hahn et al.. Response to Cervical Medial Branch Blocks In Patients with Cervicogenic Vertigo. Pain physician 2018. 21:285-294. PMID: 29871373.
- ↑ 3.0 3.1 Li & Peng. Pathogenesis, Diagnosis, and Treatment of Cervical Vertigo. Pain physician 2015. 18:E583-95. PMID: 26218949.
- ↑ Magnusen 2006
- ↑ Brandt & Huppert. A new type of cervical vertigo: Head motion-induced spells in acute neck pain. Neurology 2016. 86:974-5. PMID: 26826207. DOI.