Vertigo and Dizziness
Cervical Vertigo
Cervical Vertigo, also known as cervicogenic vertigo or cervicogenic dizziness is a controversial entity. There is evidence that it is a distinct disorder but there is no agreed upon pathophysiology, reliable test, or diagnostic criteria. Reliable and well established tests support an alternative diagnosis in almost all patients with vertigo. [1] In centres with advanced capabilities for assessing vertigo, cervical vertigo is rare. However in settings of neck trauma, dizziness is common.
All clinical studies on the condition have three major weak points: inability to confirm the diagnosis, no specific laboratory test, and unexplained discrepancy between those with severe neck pain with no vertigo and those with moderate neck pain with severe vertigo.[1]
Causes
There are multiple models that attempt to explain cervical dizziness, and they are discussed in the sections below.
Abnormal Sensory Input
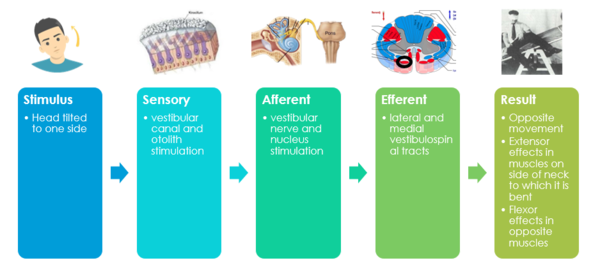
The Vestibulospinal reflex is a system for maintaining balance, posture, and, stability. When you close your eyes, the to and fro swaying is the vestibulospinal system righting the body. Some authors further subdivide the terminology and say that the vestibulospinal reflex is for muscles below the neck, and the vestibulochollic reflex if for the neck muscles. There is no objective test for detecting deficient or excessive vestibulospinal activity.
Cervical facet joints densely innervated, 50% of all cervical proprioceptors in joint capsules C1-C3. There are dense mechanoreceptors in the gamma-muscle spindles of deep segmental upper cervical muscles. Mechanoreceptor function can be altered by pain, trauma, fatigue, degeneration. There are direct connections to the vestibular and visual systems.[1]
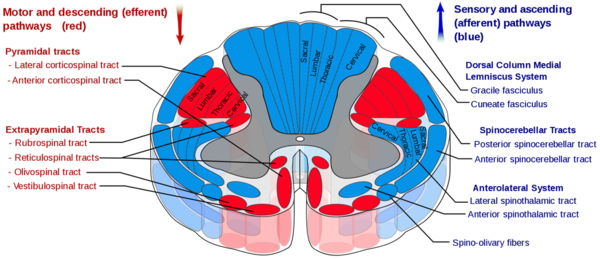
The vestibulospinal tract is a descending motor pathway (extrapyramidal) that gives motor commands that control posture. The medial tract is for neck muscles, head stabilisation / coordination, and eye movement. The lateral tract is for antigravity muscles, the leg extensors for upright posture.
There are multiple sources of indirect evidence for abnormal sensory inputs in cervical dizziness.
- Noxious stimulation of posterior neck muscles (such as vibration) can cause dizziness
- Local anaesthetic injections to upper cervical nerves or muscles can cause dizziness.
- Whiplash leads to deficits in neck position sense.
- There may be relief of vertigo with a medial branch block in whiplash.[2]
- Manual therapy seems to be effective.[3]
- There is often a disturbance in vestibulospinal control of optokinetic pursuit: Eye pursuit normal with static head, abnormal with head rotation.
Cervical vertigo may result from a sensory mismatch between vestibular and cervical inputs, with altered input form the upper cervical proprioceptors to the vestibular nuclei.[1] In whiplash cervical input may be dominant over vestibular with neck activation when there is pain or stiffness.[4] The neural mismatch model describes a mismatch between centrally expected and actual neck movement From neck pain/stiffness, inducing motion sickness. [5]
Cervical Cord Compression
Cervical cord compression or abutment, such as occurring following whiplash, can cause dizziness with or without pain. It is theorised that there is compression of the ascending or descending tracts that interact with the vestibular and cereballar systems.[6]
Rotational Vertebral Artery Occlusion
Also known as bow-hunters syndrome, this condition is rare and very difficult to diagnose. There is reversible vascular insufficiency from compression at the C1/2 junction with contraversive head movement. The dizziness may only come on after many seconds. Dissection, spasm, and stenosis of a vertebral artery can also cause dizziness.[7]
Sympathetic Dysfunction
The so-called Barré – Liéou lesion describes impingement or stimulation of the cervical sympathetic plexus causing reflex vasoconstriction of the vertebrobasilar system. Symptoms include vertigo, tinnitus, headache, blurred vision, dilated pupils, nausea. This is a controversial diagnosis, that is not supported by experimental evidence.[6]
Migraine Associated Cervicogenic Vertigo
Cervical vertigo patients overlap considerably with migraine. It is thought that neck pain can stimulate migraine, and thereby lead to dizziness. Vestibular migraine is the second most common cause of vertigo after BPPV. Migraine could be a link between cervical pain and vertigo through connections between the vestibular and trigeminal nuclei.[1][6]
Spontaneous Intracranial Hypotension
There is classically a daily orthostatic headache. The headache worsens with upright positioning, and improves when supine. It often starts abruptly. The pain may be felt in the entire head, or more localised in the bifrontal, occipital, or upper cervical regions. A significant minority of patients do not have an orthostatic headache. Associated symptoms include tinnitus, photophobia, phonophobia, dizziness, nausea and vomiting, and difficulty hearing. The condition is sometimes described in association with migraine, POTS, and Ehlers-Danlos syndrome. [8]
There are three subtypes making up three quarters of causes[8]. The remaining one quarter are indeterminate. The three types are
- Dural tear often from a ventral osteophyte that leads to an extradural CSF collection
- Nerve root diverticulum that leaks causing extradural fluid collection
- Fistula connecting the CSF to the venous system without extradural fluid collection.
As part of the assessment one should check for hypermobility using the Beighton scoring system. Measure the opening pressure, but only 34% with confirmed spinal CSF leaks were found to have a CSF pressure of ≤60 mm H2O. MRI imaging of the brain will show findings in most cases, but may be normal in chronic leaks.[8]
The epidural blood patch is the mainstay of treatment.[8]
Assessment
There is no validated method of assessment or diagnosis
History
- History of neck injury
- Pain in back of neck, radiates temporo-parietally, may only be present with palpation
- Symptoms worse with neck pain and neck movement
- Symptoms better with interventions that relieve neck pain
- Vertigo lasts minutes to hours
Examination
- Reproducible vertigo with neck manipulation
- +/- weak nystagmus that does not change with gravity, but rather with head on neck position (wait 30 seconds)
- Tender suboccipitally, C1 and C2 transverse processes
- Tender C2 and C3 spinous processes
- Tender myofascial structures
- Restricted upper C-spine range of motion
Diagnosis
There is no agreed criteria for diagnosis of cervical vertigo.
Treatment
Both Mulligan (in the form of cervical SNAGs) and Maitland mobilisations appear to be beneficial.[3]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Li & Peng. Pathogenesis, Diagnosis, and Treatment of Cervical Vertigo. Pain physician 2015. 18:E583-95. PMID: 26218949.
- ↑ Hahn et al.. Response to Cervical Medial Branch Blocks In Patients with Cervicogenic Vertigo. Pain physician 2018. 21:285-294. PMID: 29871373.
- ↑ 3.0 3.1 Li & Peng. Pathogenesis, Diagnosis, and Treatment of Cervical Vertigo. Pain physician 2015. 18:E583-95. PMID: 26218949.
- ↑ Magnusen 2006
- ↑ Brandt & Huppert. A new type of cervical vertigo: Head motion-induced spells in acute neck pain. Neurology 2016. 86:974-5. PMID: 26826207. DOI.
- ↑ 6.0 6.1 6.2 https://dizziness-and-balance.com/disorders/central/cervical/cervical.html
- ↑ Choi et al.. Rotational vertebral artery occlusion: mechanisms and long-term outcome. Stroke 2013. 44:1817-24. PMID: 23696552. DOI.
- ↑ 8.0 8.1 8.2 8.3 Grief et al. Spontaneous intracranial hypotension. Practical Neurology. May 2020. Full Text