Abdominal Cutaneous Nerve Entrapment (ACNES) Injection: Difference between revisions
From WikiMSK
No edit summary |
|||
| Line 46: | Line 46: | ||
Advised to keep active within pain limits, and is reassessed about 10 days later. Repeated injections may be performed | Advised to keep active within pain limits, and is reassessed about 10 days later. Repeated injections may be performed | ||
[[Category:Procedures]] | [[Category:Abdominal Procedures]] | ||
[[Category:Abdominal Wall]] | [[Category:Abdominal Wall]] | ||
==References== | ==References== | ||
Revision as of 15:42, 20 June 2020
Various authors have described a technique for performing an ACNE block [1][2]
Equipment
| Syringe | Needle | Steroid | Local Anaesthetic | Total Volume |
| 10mL | 25G 38mm | optional 10mg triamcinolone | Clinician choice | 10mL |
Technique
- First locate the point of maximal tenderness using the Carnett Sign
- Position: Supine
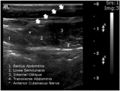
- Ultrasound Anatomy
- Transverse plane in the midline at first to identify the rectus abdominis muscle and linea alba (the medial border of the rectus abdominis).
- Move the transducer laterally to view the lateral border of the rectus abdominis and the linea semilunaris
- The target abdominal cutaneous nerve normally exits between the rectus abdominis and linea semilunaris.
- Advance the needle lateral to medial in plane
- Aspirate to ensure needle not penetrated a blood vessel.
- Inject local anaesthetic +/- steroid around the nerve
Indications
Anterior Cutaneous Nerve Entrapment Syndrome
Risks
Infection, subcutaneous injection, allergic reaction, intravascular injection ADR from steroids
Aftercare
Advised to keep active within pain limits, and is reassessed about 10 days later. Repeated injections may be performed
References
- ↑ Hong MJ, Kim YD, Seo DH. Successful treatment of abdominal cutaneous entrapment syndrome using ultrasound guided injection. Korean J Pain. 2013;26(3):291-294. doi:10.3344/kjp.2013.26.3.291
- ↑ Misoon Lee, Yong-Ik Kim, Woobin Kang. Diagnosis and Treatment of Abdominal Cutaneous Nerve Entrapment Syndrome Using Ultrasonography. Soonchunhyang Medical Science (SMS) 2016; 22(2): 147-150