Caudal Epidural Steroid Injection: Difference between revisions
No edit summary |
No edit summary |
||
| Line 11: | Line 11: | ||
==Anatomy== | ==Anatomy== | ||
[[File:Sacrum_and_Coccyx.jpg|400px]] | [[File:Sacrum_and_Coccyx.jpg|400px]] | ||
The sacrum has five fused vertebrae and has a dorsal convex curve. The [[Coccyx Anatomy|coccyx]] has three to five rudimentary vertebral bones, with a base that attaches to the sacrum, and a triangular shape. The sacrococcygeal joint is bounded by the sacrococcygeal ligament. This ligament extends dorsally in the midline and covers the sacral hiatus. | |||
==Ultrasound Guided | The sacral hiatus sits between the sacral cornua. The sacral hiatus is a natural partial defect that arises from the union of the dorsal midline of the S4 and S5 vertebrae. The floor of the sacral hiatus is the S5 vertebral body. It contains the filum terminale and coccygeal nerve. | ||
There are two sets of foramen in the sacrum. These are the four posterior sacral foramina and the four anterior sacral foramina. The sacrum attaches laterally to the bilateral ilia through the sacroiliac joints. It attaches superiorly to the L5 vertebra through the superior articular facets of the L5/S1 facet joints and through the L5/S1 disc. | |||
The sacral canal contains the epidural venous plexus that extends down to the S4 level, and is concentrated in the anterior wall of the sacral canal. It also contains epidural fat. The thecal sac generally terminates at the lower border of the S1 foramen in adults and S3 foramen in children. The PSIS is at the level of S2. Thecal sac puncture should be avoided.<ref name="Ogoke"/> | |||
==Indications and Efficacy== | |||
Good evidence for radicular leg pain due to lumbar disc herniation. 72.5% complete or partial pain relief at 12 weeks in those with symptom duration of 4-52 weeks. Fair evidence for axial pain and spinal stenosis and post surgery syndrome | |||
==Contraindications== | |||
The following are factors that predispose to dural puncture in caudal epidural injections.{{#pmid:16906188|Ogoke}} | |||
*Short stature (height less than 5 feet) | |||
*Short sagittal dimension of the sacrum | |||
*Blind injection without imaging guidance | |||
*Inexperienced operator | |||
*Tip of the needle above the level of the anterior foramen of S1 in AP view on fluoroscopy | |||
*Atypical anatomy within the sacral canal, including presence of a tethered cord. | |||
The following are potential causes of difficulty entering the caudal epidural space.Ogoke<ref name="reuse reference name"/> | |||
*Acute angle of sacral dorsal convexity | |||
*Inability to identify anatomic landmarks | |||
*Severe to morbid obesity blocking radiologic (flouroscopic) visualisation | |||
*Deformity of sacral coccygeal area secondary to previous | |||
*Trauma or birth defect | |||
*Sealed sacra; hiatus (rare) | |||
*Relatively long coccyx with “superior” location of sacral hiatus | |||
*Developmental fusion of sacral canal | |||
==Technique== | |||
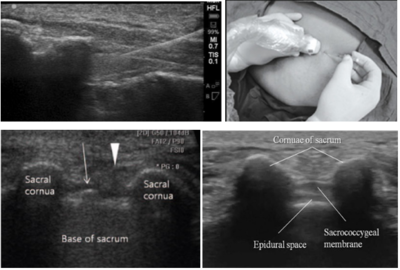
===Ultrasound Guided=== | |||
[[File:Caudal Epidural Injection Ultrasound.PNG|400px]] | [[File:Caudal Epidural Injection Ultrasound.PNG|400px]] | ||
| Line 23: | Line 52: | ||
* Aspirate to ensure needle not penetrated thecal sac or blood vessel. If aspirate CSF then abort procedure and retry in one week. | * Aspirate to ensure needle not penetrated thecal sac or blood vessel. If aspirate CSF then abort procedure and retry in one week. | ||
== | ===Landmark Guided=== | ||
*Find and mark cornuae | *Find and mark cornuae | ||
*Infiltrate lidocaine to overlying soft tissue | *Infiltrate lidocaine to overlying soft tissue | ||
| Line 31: | Line 59: | ||
*Monitor (IV access?) Empty bladder | *Monitor (IV access?) Empty bladder | ||
== | ===Fluoroscopic Guidance=== | ||
== | ==Complications== | ||
Infection, subcutaneous injection, spinal cord infarction, Radiculopathy <1:2,000 paraplegia 1:50,000, allergic reaction, intravascular injection (minimal risks with dexamethasone due to small particulate size), dural puncture with headache, PE, ADR from steroids, increased back pain (3.1%) | Infection, subcutaneous injection, spinal cord infarction, Radiculopathy <1:2,000 paraplegia 1:50,000, allergic reaction, intravascular injection (minimal risks with dexamethasone due to small particulate size), intra-osseous injection and subsequent [[Local Anaesthetic Toxicity]], dural puncture with headache, PE, ADR from steroids, increased back pain (3.1%) | ||
==Aftercare== | ==Aftercare== | ||
| Line 47: | Line 74: | ||
{{Reliable sources|synonym1="Caudal Epidural"}} | {{Reliable sources|synonym1="Caudal Epidural"}} | ||
[[Category:Lumbar Spine Procedures]] | [[Category:Lumbar Spine Procedures]] | ||
Revision as of 17:31, 19 June 2021
| Caudal Epidural Steroid Injection | |
|---|---|
| Indication | Radicular leg pain |
| Syringe | 20mL |
| Needle | 21G 40mm, or 25G 50mm |
| Steroid | Must be dexamethasone, 15mg |
| Local | No local, add normal saline |
| Volume | L5: 10mL L3: 15mL Upper lumbar: 20mL |
Anatomy
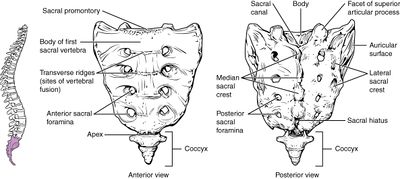 The sacrum has five fused vertebrae and has a dorsal convex curve. The coccyx has three to five rudimentary vertebral bones, with a base that attaches to the sacrum, and a triangular shape. The sacrococcygeal joint is bounded by the sacrococcygeal ligament. This ligament extends dorsally in the midline and covers the sacral hiatus.
The sacrum has five fused vertebrae and has a dorsal convex curve. The coccyx has three to five rudimentary vertebral bones, with a base that attaches to the sacrum, and a triangular shape. The sacrococcygeal joint is bounded by the sacrococcygeal ligament. This ligament extends dorsally in the midline and covers the sacral hiatus.
The sacral hiatus sits between the sacral cornua. The sacral hiatus is a natural partial defect that arises from the union of the dorsal midline of the S4 and S5 vertebrae. The floor of the sacral hiatus is the S5 vertebral body. It contains the filum terminale and coccygeal nerve.
There are two sets of foramen in the sacrum. These are the four posterior sacral foramina and the four anterior sacral foramina. The sacrum attaches laterally to the bilateral ilia through the sacroiliac joints. It attaches superiorly to the L5 vertebra through the superior articular facets of the L5/S1 facet joints and through the L5/S1 disc.
The sacral canal contains the epidural venous plexus that extends down to the S4 level, and is concentrated in the anterior wall of the sacral canal. It also contains epidural fat. The thecal sac generally terminates at the lower border of the S1 foramen in adults and S3 foramen in children. The PSIS is at the level of S2. Thecal sac puncture should be avoided.[1]
Indications and Efficacy
Good evidence for radicular leg pain due to lumbar disc herniation. 72.5% complete or partial pain relief at 12 weeks in those with symptom duration of 4-52 weeks. Fair evidence for axial pain and spinal stenosis and post surgery syndrome
Contraindications
The following are factors that predispose to dural puncture in caudal epidural injections.[1]
- Short stature (height less than 5 feet)
- Short sagittal dimension of the sacrum
- Blind injection without imaging guidance
- Inexperienced operator
- Tip of the needle above the level of the anterior foramen of S1 in AP view on fluoroscopy
- Atypical anatomy within the sacral canal, including presence of a tethered cord.
The following are potential causes of difficulty entering the caudal epidural space.Ogoke[2]
- Acute angle of sacral dorsal convexity
- Inability to identify anatomic landmarks
- Severe to morbid obesity blocking radiologic (flouroscopic) visualisation
- Deformity of sacral coccygeal area secondary to previous
- Trauma or birth defect
- Sealed sacra; hiatus (rare)
- Relatively long coccyx with “superior” location of sacral hiatus
- Developmental fusion of sacral canal
Technique
Ultrasound Guided
- Position: prone with heels rotated laterally, and a cushion pillow is used as an iliac wedge.
- Identify sacral cornua at base of imaginary triange with thumb (needle will go between cornua)
- Obtain a transverse image for the sacral hiatus and dorsal sacrococcygeal ligament between the bilateral sacral cornua,
- Obtain a longitudinal view and advance needle at a 45 degree angle.
- Terminate needle advancement right after piercing the sacrococcygeal ligament. This is to avoid injection into the venous plexus and intrathecal injection in those with unusually low terminating dural sacs.
- Aspirate to ensure needle not penetrated thecal sac or blood vessel. If aspirate CSF then abort procedure and retry in one week.
Landmark Guided
- Find and mark cornuae
- Infiltrate lidocaine to overlying soft tissue
- Enter at midline, feel it penetrate the membrane, aspirate, slow i.e. over 10 mins inject contents
- Assess post procedure for improvement in provocative manoeuvres such as SLR and pain
- Monitor (IV access?) Empty bladder
Fluoroscopic Guidance
Complications
Infection, subcutaneous injection, spinal cord infarction, Radiculopathy <1:2,000 paraplegia 1:50,000, allergic reaction, intravascular injection (minimal risks with dexamethasone due to small particulate size), intra-osseous injection and subsequent Local Anaesthetic Toxicity, dural puncture with headache, PE, ADR from steroids, increased back pain (3.1%)
Aftercare
Monitor for allergy. Advised to keep active within pain limits, and is reassessed about 10 days later. Steroid remains in situ for about 2 weeks. Up to 3-4 injections may be performed before declaring the therapy a failure. Max 0.6mg/kg or 40mg dexamethasone per year.
Videos
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,