Causes and Sources of Chronic Low Back Pain: Difference between revisions
| Line 6: | Line 6: | ||
The ''source'' of the pain refers to the anatomical structure which has nociceptive activity leading to pain perception. The ''cause'' of the pain is the disease process or disorder that is responsible for the nociceptive activity. The most well established causes of chronic low back pain are the lumbar intervertebral discs, and the lumbar zygapophysial joints. | The ''source'' of the pain refers to the anatomical structure which has nociceptive activity leading to pain perception. The ''cause'' of the pain is the disease process or disorder that is responsible for the nociceptive activity. The most well established causes of chronic low back pain are the lumbar intervertebral discs, and the lumbar zygapophysial joints. | ||
== Non-Specific Low Back Pain (~10%) == | == Non-Specific Low Back Pain (~10%) == | ||
It is often incorrectly stated that the cause of low back pain cannot be diagnosed in 85% of cases with exact figure differing with different publications (some say 80%, some say 90%)<ref>Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021 May 29;397(10289):2098-2110. doi: 10.1016/S0140-6736(21)00392-5. PMID: 34062144.</ref> This "convenient truth" has been proven to be false time and time again. Unlike acute low back pain where the causes are largely ''unknown'', '''The causes of chronic low back pain are largely ''known'''''. History and | {{Main|Non-Specific Chronic Low Back Pain}} | ||
It is often incorrectly stated that the cause of low back pain cannot be diagnosed in 85% of cases with exact figure differing with different publications (some say 80%, some say 90%)<ref>Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021 May 29;397(10289):2098-2110. doi: 10.1016/S0140-6736(21)00392-5. PMID: 34062144.</ref> This "convenient truth" has been proven to be false time and time again. Unlike acute low back pain where the causes are largely ''unknown'', '''The causes of chronic low back pain are largely ''known'''''. History, examination, and radiography are insufficient for diagnosis, but the cause can be established with at least moderate certainty in around 90% of cases as long as there is access to appropriate investigations and the investigations are done in a logical manner.<ref>{{#pmid:21266006}}</ref><ref>{{#pmid:21481166}}</ref><ref>{{#pmid:22390231}}</ref><ref>{{#pmid:21958329}}</ref><ref name=":0">{{#pmid:26218010}}</ref> | |||
==Red Flags== | ==Red Flags== | ||
Red flag conditions, such as tumours and infections are uncommon, if not rare causes | Red flag conditions, such as tumours and infections are uncommon, if not rare causes | ||
Revision as of 06:05, 7 September 2021
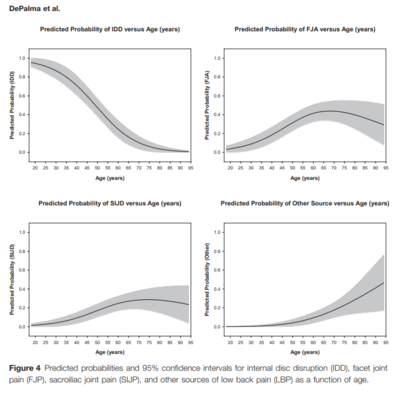
While The causes of acute low back pain are largely unknown, this is not the case for chronic low back pain, where a biomedical diagnosis is possible in the majority of cases. The exact figures depend on the age, but around 40% have disc pain, around 30% have facet joint pain, and around 20% have sacroiliac joint pain.[2]
Definitions
The source of the pain refers to the anatomical structure which has nociceptive activity leading to pain perception. The cause of the pain is the disease process or disorder that is responsible for the nociceptive activity. The most well established causes of chronic low back pain are the lumbar intervertebral discs, and the lumbar zygapophysial joints.
Non-Specific Low Back Pain (~10%)
- Main article: Non-Specific Chronic Low Back Pain
It is often incorrectly stated that the cause of low back pain cannot be diagnosed in 85% of cases with exact figure differing with different publications (some say 80%, some say 90%)[3] This "convenient truth" has been proven to be false time and time again. Unlike acute low back pain where the causes are largely unknown, The causes of chronic low back pain are largely known. History, examination, and radiography are insufficient for diagnosis, but the cause can be established with at least moderate certainty in around 90% of cases as long as there is access to appropriate investigations and the investigations are done in a logical manner.[4][5][6][7][8]
Red Flags
Red flag conditions, such as tumours and infections are uncommon, if not rare causes P% = prevalence of a serious condition in patients with acute back pain Z% = of these patients above, develops chronic back pain Prevalence of serious condition in patients that develop chronic lower back pain = (P/Z)% Eg tumours: P=1%, If 30% of acute patients become chronic, prev in chronic = (1/30)% = 3%
Lumbar Intervertebral Discs
Internal Disc Disruption
- See also: Internal Disc Disruption
Internal disc disruption is a condition that affects lumbar intervertebral discs and is the cause of pain in around 40% of individuals with chronic low back pain. The inciting event is fatigue failure of the vertebral endplate, which leads to degradation of the nuclear matrix. Subsequently radial and circumferential fissures develop that penetrate from the nucleus pulposus through to the anulus fibrosus, however the outer anulus is not breached. Pain is thought to arise through chemical nociception around the fissures ,as well as through mechanical nociception from the degraded nuclear matrix leading to greater loads being placed on the posterior anulus fibrosus.
Internal disc disruption can be diagnosed through special tests.
Disc Degeneration
Internal disc disruption is a separate concept to disc degeneration. While there are many similar processes and features, internal disc disruption is a response to injury that occurs either through single or repetitive compressive loads.[9]
Discitis
Chemical nociception can occur with irritation of the nociceptive fibres of an infected disc, and this is a red flag condition.
A disputed cause is chronic low grade infection by Propionibacterium acnes. The hypothesis is that vertebral marrow/endplate oedema caused by low grade bacterial discitis
Some studies have isolated Cutibacterium (Propionibacterium) acnes from discs in people undergoing spinal surgery. A systematic review attempted to clarify this and found that this may be related to abnormal discs being more susceptible to infection, but it is difficult to establish true infection versus contamination (some studies also isolated CONS).[10]
In an RCT of 144 patients, there was significant improvement with 100 days of augmentin in chronic low back pain, prior disc herniation, and type 1 Modic changes. Limitations included high proportions of participants having had previous back surgery, no improvement in the control group, and unclear efficacy of blinding.[11]
A multi-centre double blinded RCT was done in an attempt to reproduce the results but it was not successful. See graphic[12]
Zygapophysial Joints
Excessive compression or torsion can lead to microfracture and capsular avulsion of the zygapophysial joints. These post-traumatic structural changes have been shown in laboratory studies and postmortem pathoanatomic studies, but not in any antemortem studies.[13]
Structural Abnormalities
Tempting, but incorrect, to attribute chronic low back pain to structural abnormalities
- Congenital
- Transitional vertebrae, non-dysjunction (congenital fusion) and spina bifida occulta occur equally commonly in asymptomatic and symptomatic individuals
- Spondylolisthesis
- Large scale epidemiological studies shown in adults – not associated with pain
- Spondylolysis
- Pars defect occur in 7% of asymptomatic population, more common in sports people
- Equally as common in asymptomatic and symptomatic
- Definitive test – anaesthetize the defect
- “stress fracture” in pars interarticularis. relief of pain with LA implies defect is source, predicts surgical success
- Spondylosis/Disc degen/facet degen/OA
- Do not constitute legitimate diagnoses of cause or source of pain
Instability
Controversial term, various definitions. Clinicians have classified instability according to nature of lesions on imaging
- Fractures and fracture dislocations
- Infections of ant elements
- Neoplasms
- Spondylolisthesis
- Degenerative
Does not require demonstration of instability in biomechanical sense
Spondylolisthesis
Spondylolithesis rarely progresses in adults Radiographic studies show that Grade 1 and 2 are associated with reduced range of motion rather than instability Further precision studies have shown that motion patterns of patients are indisguishable from degenerative disc disease
Degeneration of the Lumbar Spine
Several types of instability have been attributed to degen of lumbar spine These include:
- Rotational – hypothetic entity, certain radiographic signs suggested, reliability/validity not est
- Retrolisthetic – during extension (but this movement can occur in asymptm)
- Translational – abnormal forward translation during flexion. Difficulty in defining upper limit of normal (3-4mm in different studies)
Despite all efforts to define – no studies have shown that it is related to cause of pain, nor rectifying it abolishes symptoms
Degenerative changes are an expression of metabolic stress, not a disease No known mechanism whereby degenerative changes can be painful Lots of different triggers, however final common pathway Degenerative joint disease is a disturbing label that patients associate with a poor prognosis Genetic factors predispose to degenerative changes, but age is the strongest correlate In contrast, features of internal disc disruption correlate strongly with back pain
Biology
- Chondrocytes maintain balance between synthesis and degradation
- Synthesis promoted by growth factors
- Degradation achieved by action of MMP, whose synthesis is activated by TNF𝛼
- Osteophytes – adaptive modelling, attempt to increase surface area to reduce load. May be normal joint, with excessive load, or joint which capacity to bear loads is compromised by degradation of matrix.
Regional Differences - Discs
- Cervical
- Differ from lumbar discs in their anatomic structure and their expression of degenerative change
- Cervical discs lack a concentric anulus fibrosus, only well developed anteriorly
- Nucleus pulposus persists until 2nd decade, changes to firm, dry fibrocartilage plate
- Changes are essential for allowing axial rotation
- Lumbar
- Degen changes are more chemical in nature, expressed as changes in PG/hydration. Seen on MRI with change in signal intensity
ZA Joints
- Cervical:
- Face upwards and backwards, therefore equally share compressive load with discs
- Injuries most likely to occur from weight bearing
- Degenerative changes occur at all levels, most commonly C3/4
- Lumbar:
- Face posteriorly and laterally, share little of the axial load
- Resists axial rotation and anterior translation
- Degenerative changes arise earlier, more common in L4/5
Causes of degenerative disc disease
Specific metabolic causes are rare
- Limited to diabetes mellitus and ochronosis
- Impaired nutrition promoted, evidence lacking
- Vascular disease, smoking weak correlate
- Low grade infection explored – not conclusive
- Strongest relationship – AGE
Aging Changes
- Chondrocytes might be subject to innate senescence
- They may have genetic abnormalities that affect matrix quality
- Or normal cells may become impaired with accum toxins/mechanical stresses
- Z joints have not been explicitly studied
- Under umbrella of synovial joints – combination of genetic factors/abnormal biomechanics
- Lumbar disc degeneration – evidence more explicit (twin studies)
- Heavy loads account for some variance
- Larger proportions explained by genetic factors
Correlations
- One method is to compare prevalence in people with and without pain. If prev is higher in people with pain, association is established
- Another method is to anesthetize joint. If relieves pain, target joint is implicated as source.
The prevalence of lumbar disc degeneration in asymptomatic individuals, clearly increases with age Radiographic features of cervical spine in asymptomatic people again increases with age (hardly any “normal” looking spines in over 50)
Neck Pain
Study compared patients with neck pain, with controls. There were no differences in prevalence of spondylosis, severe disc changes or facet joint changes between cases and controls. Degenerative changes in cervical discs/z joints do not correlate with pain
Low Back Pain
A large population study looked at osteoarthosis in the context of pain No association with pain, irrespective of grade Many studies on disc degeneration Systematic reviews on high quality studies showed no clinical association between degenerative disc changes and pain
Spondylolisthesis
- Spondylolithesis – translation of 1 vertebral body on another. 6 broad categories – (wiltse classification) isthmic, traumatic, degen, pathologic, dysplastic and post surgical. It can also be classified according to severity (Merding)
- Bogduk – not associated with pain, finding it on xray does not constitute diagnosis. Rarely progresses. Grade 1 – 2 associate with reduced ROM rather than instability.
Degenerative Lumbar Spondylolisthesis
- Incidence 19-43%, mean age 71, most common in females
- Most common L4/5
- Initial event – disc degeneration/narrowing of disc space - micro-instability
- Cause of pain multi factorial
- Most are grade 1 (75%) – less than 25% slip
- Average slip progression – 18%, no correlation between progression and symptoms
- Natural history and management of low grade slip is controversial, conservative management generally indicated. Surgery for refractory cases
Isthmic Lumbar Spondylolisthesis
- Isthmic meaning movement of one vertebrae on another, due to a defect in the pars, termed spondylolysis (unhealed stress fracture). Spondylolysis can be present without displacement. Spondylolistesis occurs in 40-60% of patients with bilateral spondylolysis (unlikely if unilateral).
- Most are asymptomatic, 25% have back/radicular pain
- Prevalence in children 2.6%, increasing to 4% in adult
- Asymptomatic in 3-11% of adults
- More common in men, L5/S1
- Causes are multifactorial, genetic component
- Back pain may be from micro-stability or pain from degenerative disc
- Symptomatic patients are initially treated non-operatively
High grade lumbar sponylolisthesis
- Defined as >50% slippage
- Most are at L5/S1, a result of isthmic spondylolisthesis
- Most have a degree of neurologic compromise
- Pain usually with hyperextension, resolves with time due to fracture union
- Treatment is focused on correction of lordosis and sagittal balance
- Natural history – difficult to predict if further slippage will occur
- Conservative management trialed in adolescence, usually unable to provide permanent relief�
Surgical vs Non Surgical Treatment of Lumbar Spondylolithesis – Karsy et al.
- Non operative effective in patients without neurogenic claudication or radiculopathy and stable spondylolisthesis (grade 1)
- 1/3 show progression over time
- Lumbar decompression alone can be effective for low grade, fusion if higher grade
- Mechanical instability is change of 3mm-6mm between flexion/ext films, or change from sitting to standing
- Meta analysis – surgical intervention is more effective than non operative, for patients with pain and functional limitations
Lumbar instability – J. Beazell
- Historical term, that has been debated through 1980-90’s
- Encompasses two types:
- Mechanical (radiographic)
- Functional (clinical)
- Topic is subject to much debate on exact nature of problem, correlation with history and relevance to patient management
Seminal Journal Articles
Degenerative Joint Disease of the Spine – N. Bogduk. Radiol Clin N Am 50 (2012) 613–628
High-Grade Lumbar Spondylolisthesis – A. Beck et al. Clin N Am 30 (2019) 291-298
Isthmic Lumbar Lumbar Spondylolisthesis – A. Bhalla. Clin N Am 30 (2019) 283-290
Degenerative Lumbar Spondylolisthesis – M. Bydon. Clin N Am 30 (2019) 299-304
Surgical vs Non Surgical Treatment of Lumbar Spondylolisthesis. Clin N Am 30 (2019) 333-340
Lumbar instability: an evolving and challenging concept. J. Beazell. Journal of Manual and Manpulative Therapy. Vol 18 1 (2010)
- ↑ DePalma MJ, Ketchum JM, Saullo T. What is the source of chronic low back pain and does age play a role? Pain Med. 2011 Feb;12(2):224-33. doi: 10.1111/j.1526-4637.2010.01045.x. Epub 2011 Jan 25. PMID: 21266006.
- ↑ DePalma MJ. Diagnostic Nihilism Toward Low Back Pain: What Once Was Accepted, Should No Longer Be. Pain Med. 2015 Aug;16(8):1453-4. doi: 10.1111/pme.12850. Epub 2015 Jul 27. PMID: 26218010.
- ↑ Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021 May 29;397(10289):2098-2110. doi: 10.1016/S0140-6736(21)00392-5. PMID: 34062144.
- ↑ DePalma et al.. What is the source of chronic low back pain and does age play a role?. Pain medicine (Malden, Mass.) 2011. 12:224-33. PMID: 21266006. DOI.
- ↑ DePalma et al.. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain medicine (Malden, Mass.) 2011. 12:732-9. PMID: 21481166. DOI.
- ↑ DePalma et al.. Multivariable analyses of the relationships between age, gender, and body mass index and the source of chronic low back pain. Pain medicine (Malden, Mass.) 2012. 13:498-506. PMID: 22390231. DOI.
- ↑ DePalma et al.. Structural etiology of chronic low back pain due to motor vehicle collision. Pain medicine (Malden, Mass.) 2011. 12:1622-7. PMID: 21958329. DOI.
- ↑ DePalma. Diagnostic Nihilism Toward Low Back Pain: What Once Was Accepted, Should No Longer Be. Pain medicine (Malden, Mass.) 2015. 16:1453-4. PMID: 26218010. DOI.
- ↑ Bogduk N, Aprill C, Derby R. Lumbar discogenic pain: state-of-the-art review. Pain Med. 2013 Jun;14(6):813-36. doi: 10.1111/pme.12082. Epub 2013 Apr 8. PMID: 23566298.
- ↑ Urquhart DM et al. Could low grade bacterial infection contribute to low back pain? A systematic review.BMC Med 2015;13:13.
- ↑ Albert H, Sorensen J, Christensen B, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy.Eur Spine J.2013;22:697–707
- ↑ Bråten LCH, Rolfsen MP, Espeland A, et al. Efficacy of antibiotic treatment in patients with chronic low back pain and Modic changes (the AIM study): double blind, randomised, placebo controlled, multicentre trial [published correction appears in BMJ. 2020 Feb 11;368:m546]. BMJ. 2019;367:l5654. Published 2019 Oct 16. doi:10.1136/bmj.l5654
- ↑ Wade King and Nikolai Bogduk. Chronic Low Back Pain In: Bonica's Management of Pain. 2018

