Cervical Radicular Pain and Radiculopathy
Definitions
- Main article: Cervical Spine Pain Definitions
Cervical radiculopathy is characterised by objective loss of neurologic function. Loss of function is some combination of sensory loss, motor loss, or impaired reflexes, in a segmental distribution. Pain is not a component of radiculopathy, and so is distinguished from cervical radicular pain.[1]
Pathophysiology
Not much is known about the causes and mechanisms of cervical radicular pain. The literature often uses the term cervical radiculopathy, but radiculopathy and radicular pain are not synonymous.
Radiculopathy arises from either direct compression of a cervical spinal nerve or root, or by ischaemia from vascular injury to their blood supply. There is a conduction block along the affected axons which results in sensory or motor loss. Compression of axons, including those of the lumbar nerve roots, does not cause activity in nociceptive afferent fibres. Meanwhile, compression of a dorsal root ganglion does cause pain through activation of Aβ and C fibres. The causes of cervical radicular pain cannot therefore be attributed to the same causes as those of radiculopathy.
It is thought that inflammation of the cervical nerve roots is the underlying mechanism through which radicular pain occurs secondary to disc herniation. There are pro-inflammatory molecules in disc material. Meanwhile, inflammation is not the cause of pain in other causes of radicular pain when due to tumours, cysts, and osteophytes. In these conditions it must be through dorsal root ganglion compression that pain occurs, as these conditions are non-inflammatory in nature.[1]
Aetiology
Clinical Features
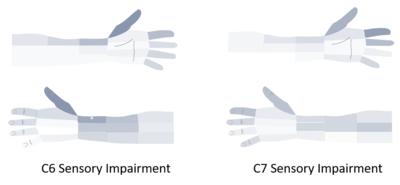
Cervical radiculopathy is characterised by negative objective signs: sensory loss, motor loss, or impaired reflexes, in a segmental distribution. The sensory loss occurs in the upper limbs, and tends to be dermatomal in distribution.[1] Notably however C6 and C7 cannot be differentiated based on dermatomes alone.[2]
The pattern of cervical radicular pain on the other hand is not dermatomal. The pain can be felt proximally in the scapula and shoulder girdle, and scapula pain usually precedes pain in the arm and/or fingers. This is analogous to the common finding of buttock pain with lumbar radicular syndrome. The reason it is not dermatomal is likely due to the pain not being restricted to cutaneous fibres, but there is also a deeper pain arising from the muscles and joints. The segmental innervation of the skin (dermatomes) is different to that of the deeper tissues. The muscles of the shoulder girdle are supplied by C6 and C7, very different to their dermatomes. And so the segmental innervation of muscles is more closely related to the radicular pain patterns than dermatomes, while dermatomes are more helpful for patterns of sensory loss in radiculopathy.[1][3]
The site of scapula pain may be a helpful data point in determining the affected level in cervical radicular pain. Mizutamari et al suspect that scapula pain occurs through the medial branches of the dorsal rami of the cervical nerves. They found that there was no cutaneous course of C6 and C7 and that these patients complained of deep scapula pain only. This is compared to patients with C5 and C8 lesions having both superficial and deep pain.[3]
| Nerve root | Shoulder Girdle Region | Deep or superficial |
|---|---|---|
| C5 | Suprascapular region | Superficial and deep pain |
| C6 | Suprascapular to posterior deltoid region | Deep pain |
| C7 | Interscapular region | Deep pain |
| C8 | Interscapular and scapular regions | Superficial and deep pain |
References
- ↑ 1.0 1.1 1.2 1.3 Bogduk. The anatomy and pathophysiology of neck pain. Physical medicine and rehabilitation clinics of North America 2011. 22:367-82, vii. PMID: 21824580. DOI.
- ↑ 2.0 2.1 Rainville et al.. Exploration of sensory impairments associated with C6 and C7 radiculopathies. The spine journal : official journal of the North American Spine Society 2016. 16:49-54. PMID: 26253986. DOI.
- ↑ 3.0 3.1 3.2 Mizutamari et al.. Corresponding scapular pain with the nerve root involved in cervical radiculopathy. Journal of orthopaedic surgery (Hong Kong) 2010. 18:356-60. PMID: 21187551. DOI.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,
![(a)C5 and C8 cutaneous nerves traverse up and down the spine of the scapula, respectively, whereas the courses of C6 and C7 cutaneous nerves are not found. (b) The site of radicular pain involving the C6 root overlaps with that of the C5 root, and also involves the posterior deltoid.[3]](/w/img_auth.php/thumb/0/0d/Cervical_radicular_scapula_pain.png/500px-Cervical_radicular_scapula_pain.png)


