Fibrous Connective Tissues: Difference between revisions
mNo edit summary |
|||
| Line 12: | Line 12: | ||
==Collagen== | ==Collagen== | ||
[[File:Tendon hierarchical organisation.jpg|thumb|The hierarchical organisation of tendons]] | [[File:Tendon hierarchical organisation.jpg|thumb|500px|The hierarchical organisation of tendons]] | ||
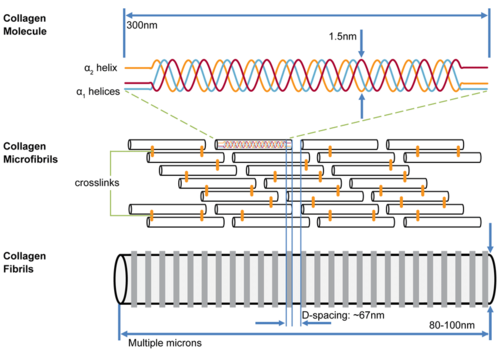
[[File:Collagen structure and organisation.png|thumb|The hierarchical organisation of collagen molecules (tropocollagen) which self-assemble in a quarter-staggered array into microfibrils to form collagen fibrils with characteristic spacing.]] | [[File:Collagen structure and organisation.png|thumb|500px|The hierarchical organisation of collagen molecules (tropocollagen) which self-assemble in a quarter-staggered array into microfibrils to form collagen fibrils with characteristic spacing.]] | ||
=== Structure === | === Structure === | ||
| Line 27: | Line 27: | ||
=== Biomechanics === | === Biomechanics === | ||
{{multiple image | |||
|perrow=2 | |||
|align=right | |||
|total_width=700px | |||
|image1=Collagen stress strain curve tendon.png | |||
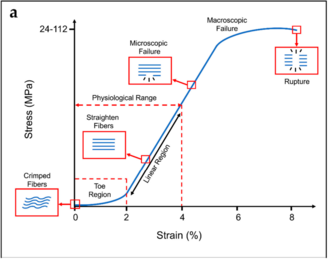
|caption1='''Tendon stress-strain curve''' (typical) {{#pmid:30322082|Sensini}} | |||
|image2=Collagen stress strain curve ligament.png | |||
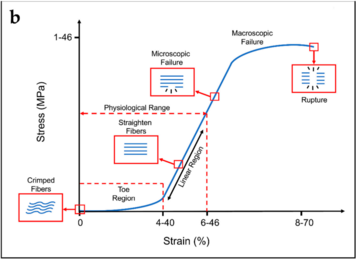
|caption2='''Ligament stress-strain curve''' (typical)<ref name="Sensini"/> | |||
|footer=Typical ranges of stress and strain are indicated on the x and y axes. | |||
|}} | |||
With stretching of a collagen fibre, the fibre resists elongation due to a resistance force from the chemical bonds between the collagen fibrils, between tropocollagen molecules, between collagen fibres, and between collagen fibres and proteoglycans. | |||
The biomechanics of collagen can be understood through the stress-strain curve. First, two key definitions: | The biomechanics of collagen can be understood through the stress-strain curve. First, two key definitions: | ||
| Line 48: | Line 59: | ||
== Proteoglycans == | == Proteoglycans == | ||
'''Structure''' | '''Structure''' | ||
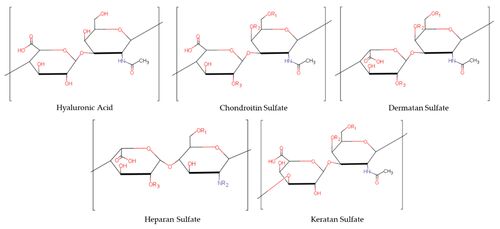
[[File:Glycosaminoglycans.jpg|thumb| | [[File:Glycosaminoglycans.jpg|thumb|500px|Repeating disaccharide unit of each glycosaminoglycan]] | ||
Proteoglycans are chains of glycosaminoglycans hanging from a core protein. Glycosaminoglycans are simply long chains of sugars, that are characterised by their repeating units. The repeating units are a pair of 6-carbon structures: a hexose (also called hexuronic acid) and a hexosamine. Hexosamines are amino sugar linked by glycosidic bonds. Different hexoses and hexosamines give rise to different glycosaminoglycans. | Proteoglycans are chains of glycosaminoglycans hanging from a core protein. Glycosaminoglycans are simply long chains of sugars, that are characterised by their repeating units. The repeating units are a pair of 6-carbon structures: a hexose (also called hexuronic acid) and a hexosamine. Hexosamines are amino sugar linked by glycosidic bonds. Different hexoses and hexosamines give rise to different glycosaminoglycans. | ||
| Line 86: | Line 97: | ||
|} | |} | ||
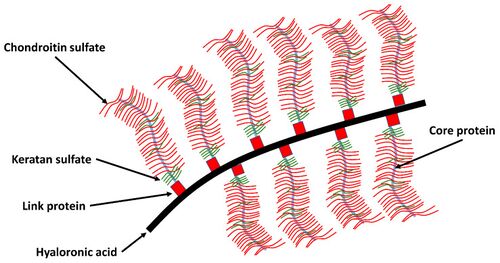
[[File:Proteoglycan network in articular cartilage.jpg|thumb| | [[File:Proteoglycan network in articular cartilage.jpg|thumb|500px|'''Aggregated Proteoglycan''': depicted as a central hyaluronic acid filament, with proteoglycans attached to it. The proteoglycans are made up of core proteins with attached glycosaminoglycans]] | ||
Glycosaminoglycans come together to stick onto a core protein through covalent bonds. Each one of these structures is a proteoglycan, bearing chondroitin-sulphate and keratan sulphate as the cardinal glycosaminoglycans. Hyaluronic acid, another glycosaminoglycans, gets together with proteoglycans to form an aggregated proteoglycan. To stabilise the aggregation, a link protein binds the head end of the core protein to the hyaluronic acid. The proteoglycan aggregate is very large. | Glycosaminoglycans come together to stick onto a core protein through covalent bonds. Each one of these structures is a proteoglycan, bearing chondroitin-sulphate and keratan sulphate as the cardinal glycosaminoglycans. Hyaluronic acid, another glycosaminoglycans, gets together with proteoglycans to form an aggregated proteoglycan. To stabilise the aggregation, a link protein binds the head end of the core protein to the hyaluronic acid. The proteoglycan aggregate is very large. | ||
Revision as of 15:38, 11 August 2021
It could be said that Musculoskeletal Medicine is the study of disorders of fibrous connective tissues. Fibrous connective tissues are those tissues that are designed to withstand mechanical deformation.
Structural Overview
Deformation comes in two principal forms, tension and compression. However there are also shear forces. To withstand tension the body forms "strings" in the form of collagens. To withstand compression the body develops a fluid "mush" in the form of proteoglycans.
The fibrous connective tissues exist in a spectrum of composition. The more a tissue is required to withstand tension the more collagen it will have, while the more it is required to withstand compression the more proteoglycans it will have.
Tendons (principally collagen) -> ligaments (principally collagen plus 0.5% proteoglycans) -> fascia (mixed collagen and proteoglycans) -> cartilage (principally proteoglycans plus some collagen) -> bone (essentially cartilage that has been doped by calcium)
These various components are synthesised by cells. Fibroblasts manufacture the components of tensile tissues. Chondroblasts produce the components of cartilage. Osteoblasts form the components of bone. These various cells can transform into one another for example ligaments can become cartilaginous and then osseous.
Collagen
Structure
The primary component of collagen is a polypeptide. The secondary structure is a helix. These helices are arranged into a tertiary structure called a triple helix. Those components are aggregated into a quaternary structures in increasing complexity: microfibrils -> fibrils -> fibres -> bundles -> fascicles
The primary functional unit of collagen is tropocollagen, which consists of a triple helix of polypeptide chains of around 1000 amino acid residues each. Tropocollagen measures around 3000 Å long by 15 Å wide.
Tropocollagen fibres aggregate end-to-end and side-to-side in a semi-overlapping pattern. The side-to-side tropocollagen fibres are joined by cross-links that occur during the normal maturation process. There is also end-to-end bonding.
One of the sources of resistance to tension is the end-to-end bonding between the polypeptide chains. Otherwise this triple helical structure when subjected to tension has the spaces between the helices taken up a little as it flattens out without being disrupted. However there is an electrical repulsion resisting this deformation.
Collagen is a very long-lived molecule with a slow rate of turnover. With normal ageing, there is an accumulation of cross-linking, which increases the stiffness and resistance to stretch.
Biomechanics
With stretching of a collagen fibre, the fibre resists elongation due to a resistance force from the chemical bonds between the collagen fibrils, between tropocollagen molecules, between collagen fibres, and between collagen fibres and proteoglycans.
The biomechanics of collagen can be understood through the stress-strain curve. First, two key definitions:
- Stress = the applied elongating force, measured in units of force (newtons)
- Strain = the extent to which a fibre is elongated, measured as the fractional or percentage increase in length relative to the initial length. A fibre of length L0 when stretched to a new length L1 undergoes a strain of L1/L0 x 100%
The stress-strain curve therefore represents the behaviour of a collagen fibre when it is subjected to a force (stress) that ventures to elongate the fibre (strain).
There are three regions of the stress-strain curve
- Toe Region: This is where the crimp is being removed from the collagen fibre with the application of stress. Crimp refers to the resting state of collagen fibres being buckled and wavy. Deformation here requires little energy due to no resistance from major chemical bonds, but not much deformation occurs at this point. The wavy fibres and transformed into straight fibres at the end of this region.
- Linear Region: The second, linear region is the steep slope along the middle of the curve. Here the stress stretches the collagen fibre longitudinally after the crimp has been removed. The bonds within and between the collagen fibrils and tropocollagen molecules are being strained and there is some micro-failure. A large amount of stress is needed for only a small amount of elongation.
- Macroscopic Failure: The last part of the curve is once macro-failure has occurred, with substantial numbers of bonds being irreversibly broken. Elongation occurs with ever decreasing amounts of stress. Collagen fibrils start to be strained and broken somewhere after 3% and 4% of elongation of the fibre. About 4% is the maximum a fibre can sustain without risking microscopic damage.
Tendons have specific load transfer functions, and the toe region of their stress-strain curve is short (2-5%), and is similar with each tendon in the body. Ligaments on the other hand allow different ranges of motion in different joints, and have wider ranges of strain for the toe region depending on the anatomical site (ACL is 4%, spine ligaments are 10-40%).[1]
Clinical examination only evaluates no further than just beyond the toe phase.
The most important property of collagen is its tensile strength. Collagen buckles when it is compressed. In articular cartilage the tensile strength properties of collagen is complementary to proteoglycans which ensure compressive strength, elasticity, and the lifespan of articular cartilage (see Synovial Joints).
Proteoglycans
Structure
Proteoglycans are chains of glycosaminoglycans hanging from a core protein. Glycosaminoglycans are simply long chains of sugars, that are characterised by their repeating units. The repeating units are a pair of 6-carbon structures: a hexose (also called hexuronic acid) and a hexosamine. Hexosamines are amino sugar linked by glycosidic bonds. Different hexoses and hexosamines give rise to different glycosaminoglycans.
The glycosaminoglycans commonly found in fibrous connective tissues are chondroitin-6-sulphate, chondroitin-4-sulphate, keratan sulphate, dermatansulphate, and hyaluronic acid. Hyaluronic acid has a significantly larger molecular weight.
In hyaluronic acid there is a carboxyl group in each pair of repeating units, and this carboxyl group can ionise. Chondroitin-4-sulphate has a carboxyl group, and a sulphate group, which are both ionisable. Similarly in chondroitin-4-sulphate, there are two ionisable radical groups. In keratan sulphate, there is only one ionisable sulphate radical. Hyaluronic acid is unsulphated.
| Glycosaminoglycan | Hexuronic acid | Hexosamine |
|---|---|---|
| Chondroitin 4 Sulphate | glucuronic Acid | N-acetylgalactosamine 4 sulphate |
| Chondroitin 6 Sulphate | glucuronic Acid | N-acetylgalactosamine 6 sulphate |
| Dermatan Sulfate | Iduronic Acid | N-acetylgalactosamine |
| Keratan Sulfate | galactose | N-acetylglucosamine |
| Heparan Sulfate | glucuronic Acid | N-acetylglucosamine |
| Hyaluronic Acid | glucuronic Acid Unsulfated | N-acetyl-D-glucosamine Unsulfated |
Glycosaminoglycans come together to stick onto a core protein through covalent bonds. Each one of these structures is a proteoglycan, bearing chondroitin-sulphate and keratan sulphate as the cardinal glycosaminoglycans. Hyaluronic acid, another glycosaminoglycans, gets together with proteoglycans to form an aggregated proteoglycan. To stabilise the aggregation, a link protein binds the head end of the core protein to the hyaluronic acid. The proteoglycan aggregate is very large.
Water Binding Potential
There is a great electrostatic capacity in this structure. The negative charges in the sulphate and the carboxyl groups are attracted to the positively charged ends of water molecules. This is one of the two key ways that the aggregated proteoglycan can bind water.
The other way that it binds water is through thermodynamic principles. Any water molecules are spontaneously moving due to its thermodynamic properties. With a free body of water all the molecules exhibit similar activity. However in the presence of proteoglycans, the physical presence slows down the activity of water, preventing its egress. The aggregated proteoglycan exists not as a straight structure, but is highly coiled.
In ageing there is an increase in the ratio of keratan sulphate to chondroitin sulphate. Keratan sulphate as above only has one ionisation group, and so the proteoglycans have relatively less charge. Therefore with ageing, as the KS:CS ratio increases, the electrostatic water binding capacity is reduced.
Synthesis
See Also
References
- ↑ 1.0 1.1 1.2 Sensini & Cristofolini. Biofabrication of Electrospun Scaffolds for the Regeneration of Tendons and Ligaments. Materials (Basel, Switzerland) 2018. 11:. PMID: 30322082. DOI. Full Text.
- ↑ Sodhi H, Panitch A. Glycosaminoglycans in Tissue Engineering: A Review. Biomolecules. 2020 Dec 29;11(1):29. doi: 10.3390/biom11010029. PMID: 33383795; PMCID: PMC7823287.