Gluteal Tendinopathy: Difference between revisions
mNo edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{ | {{Authors|Authors=EmilyG|Peer reviewer=Jeremy|Additional contributors=Jeremy}} | ||
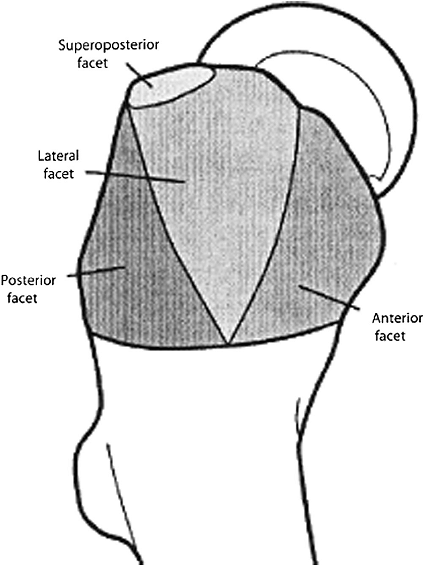
Greater trochanteric pain syndrome (GTPS) | {{Condition|quality=Partial|image=Greater trochanter facets.png|caption=The facets of a right greater trochanter. The [[Gluteus Medius|gluteus medius]] inserts at the superoposterior and lateral facets; [[Gluteus Minimus|gluteus minimus]] inserts at the anterior facet.}} | ||
==Aetiology and Pathophysiology == | Greater trochanteric pain syndrome (GTPS) is an umbrella term encompassing different musculoskeletal entities that may contribute to chronic lateral hip pain. Tendinopathy of gluteus medius and/or gluteus minimus is the most common cause of GTPS and is generally simply referred to as gluteal tendinopathy. Other causes of GTPS are [[Snapping Hip Syndrome|coxa saltans (snapping hip)]] with disorders of tensor fascia lata and/or the iliotibial band, and trochanteric bursitis. However, any inflamed or enlarged bursa seen (sub-gluteal minimus/medius) is invariably secondary to or co-exists with an underlying gluteal tendinopathy. Therefore the terms "trochanteric bursitis" and "trochanteritis" are generally regarded as misnomers. | ||
== Anatomy == | |||
In the "rotator cuff of the hip" there are six external rotators and three internal rotators. | |||
*The external rotators are [[piriformis]], [[Gemelli Muscles|gemellus superior and inferior]], [[Obturator Internus|obturator internus]], [[Obturator Externus|obturator externus]], and [[Quadratus Femoris|quadratus femoris]]. | |||
*The internal rotators are [[Gluteus Minimus|gluteus minimus]], [[Gluteus Medius|gluteus medius]], and [[Tensor Fascia Lata|tensor fascia lata]]. | |||
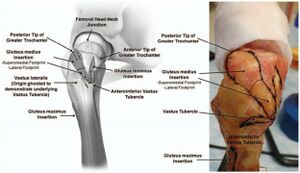
[[Gluteus Medius|Gluteus medius]] is a large fan-shaped muscle that has its origin at the outer edge of the iliac crest running from the anterior superior iliac spine (ASIS) to the posterior superior iliac spine (PSIS). It has three equal portions: anterior, middle, and posterior. The anterior and middle portions assist with initiating hip abduction. The posterior portion is active in heel strike to full stance during gait to stabilise the hip. It inserts at the superoposterior and lateral facets of the greater trochanter. | |||
<gallery widths=300px heights=300px> | |||
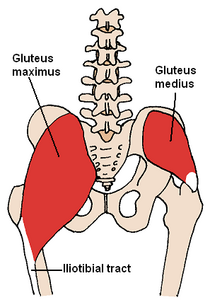
File:Posterior_Hip_Muscles_2.png|gluteus medius shown on the right | |||
File:Posterior Hip Muscles_1.PNG|gluteus minimus shown on the right | |||
File:Lateral hip illustration and cadaver.jpg|lateral hip with foot prints of gluteus medius, gluteus minimus, and vastus lateralis | |||
</gallery> | |||
==Aetiology and Pathophysiology== | |||
Gluteal tendinopathy is caused by exposure to load that the tendon did not have adequate adaption or recovery time in order manage.<ref name=":1">{{Cite journal|last=Grimaldi|first=Alison|last2=Mellor|first2=Rebecca|last3=Hodges|first3=Paul|last4=Bennell|first4=Kim|last5=Wajswelner|first5=Henry|last6=Vicenzino|first6=Bill|date=2015-05-13|title=Gluteal Tendinopathy: A Review of Mechanisms, Assessment and Management|url=http://dx.doi.org/10.1007/s40279-015-0336-5|journal=Sports Medicine|volume=45|issue=8|pages=1107–1119|doi=10.1007/s40279-015-0336-5|issn=0112-1642}}</ref><ref name=":2">{{Cite journal|last=Cook|first=J L|last2=Purdam|first2=C R|date=2008-09-23|title=Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy|url=http://dx.doi.org/10.1136/bjsm.2008.051193|journal=British Journal of Sports Medicine|volume=43|issue=6|pages=409–416|doi=10.1136/bjsm.2008.051193|issn=0306-3674}}</ref> This could be due to a traumatic event (e.g. direct blow) or a frequent and repeated exposure to a load (e.g. jumping athlete).<ref name=":2" /><ref name=":1" /> Three continuous stages of disease have been described: normal to reactive tendinopathy to tendon dysrepair to degenerative tendinopathy.<ref name=":1" /> This is explained in more detail in [[Tendinopathy]]. It is difficult because pain is not closely connected to progression of pathology.<ref name=":2" /> | Gluteal tendinopathy is caused by exposure to load that the tendon did not have adequate adaption or recovery time in order manage.<ref name=":1">{{Cite journal|last=Grimaldi|first=Alison|last2=Mellor|first2=Rebecca|last3=Hodges|first3=Paul|last4=Bennell|first4=Kim|last5=Wajswelner|first5=Henry|last6=Vicenzino|first6=Bill|date=2015-05-13|title=Gluteal Tendinopathy: A Review of Mechanisms, Assessment and Management|url=http://dx.doi.org/10.1007/s40279-015-0336-5|journal=Sports Medicine|volume=45|issue=8|pages=1107–1119|doi=10.1007/s40279-015-0336-5|issn=0112-1642}}</ref><ref name=":2">{{Cite journal|last=Cook|first=J L|last2=Purdam|first2=C R|date=2008-09-23|title=Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy|url=http://dx.doi.org/10.1136/bjsm.2008.051193|journal=British Journal of Sports Medicine|volume=43|issue=6|pages=409–416|doi=10.1136/bjsm.2008.051193|issn=0306-3674}}</ref> This could be due to a traumatic event (e.g. direct blow) or a frequent and repeated exposure to a load (e.g. jumping athlete).<ref name=":2" /><ref name=":1" /> Three continuous stages of disease have been described: normal to reactive tendinopathy to tendon dysrepair to degenerative tendinopathy.<ref name=":1" /> This is explained in more detail in [[Tendinopathy]]. It is difficult because pain is not closely connected to progression of pathology.<ref name=":2" /> | ||
| Line 12: | Line 26: | ||
===Examination=== | ===Examination=== | ||
The most important sign is pain on palpation of the greater trochanter. | The patient is assessed during [[gait]] to evaluate for a Trendelenburg pattern. | ||
The most important sign is pain on palpation of the greater trochanter. Absence of pain on palpation would indicate an alternate diagnosis.<ref name=":1" /> | |||
Lateral hip pain reproduced on 30s single-leg stance test was a sensitivity and specificity of 100% and 97.3% respectively for gluteal tendinopathy. The high utility of the test is only maintained if lateral displacement of the hip is avoided. The examiner may provide gentle fingertip support to steady the patient.<ref name=":1" /> | |||
The FABER test is useful in the differential diagnosis as limited range of movement is associated with hip joint pathology but not gluteal tendinopathy.<ref name=":1" /> | |||
The Ober's test has been shown to lack diagnostic utility for gluteal tendinopathy.<ref name=":1" /> | |||
The resisted internal rotation test had a sensitivity of 92% and specificity of 85% for the detection of gluteus medius tears. | |||
==Investigations== | ==Investigations == | ||
MRI is gold standard as it can visualise changes associated with gluteal tendinopathy, such as tendon thickening and soft tissue oedema, the clearest.<ref name=":1" /> MRI is also useful in excluding other causes of lateral hip pain.<ref name=":1" /> However, MRI is expensive and not very accessible.<ref name=":1" /> Consequently, ultrasound is typically used in clinical practice.<ref name=":1" /> The accuracy of ultrasound in identifying gluteal tendinopathy is variable and dependent on operator experience and patient characteristics.<ref name=":1" /> It is important to note that it is normal for radiological changes to be present in the asymptomatic population, thus, any findings need to be considered within the clinical context.<ref name=":1" /> | MRI is gold standard as it can visualise changes associated with gluteal tendinopathy, such as tendon thickening and soft tissue oedema, the clearest.<ref name=":1" /> MRI is also useful in excluding other causes of lateral hip pain.<ref name=":1" /> However, MRI is expensive and not very accessible.<ref name=":1" /> Consequently, ultrasound is typically used in clinical practice.<ref name=":1" /> The accuracy of ultrasound in identifying gluteal tendinopathy is variable and dependent on operator experience and patient characteristics.<ref name=":1" /> It is important to note that it is normal for radiological changes to be present in the asymptomatic population, thus, any findings need to be considered within the clinical context.<ref name=":1" /> | ||
| Line 20: | Line 44: | ||
<u>Grey scale Ultrasound</u><ref name=":3">{{Cite journal|last=Kong|first=Andrew|last2=Van der Vliet|first2=Andrew|last3=Zadow|first3=Steven|date=2006-12-06|title=MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome|url=http://dx.doi.org/10.1007/s00330-006-0485-x|journal=European Radiology|volume=17|issue=7|pages=1772–1783|doi=10.1007/s00330-006-0485-x|issn=0938-7994}}</ref> | <u>Grey scale Ultrasound</u><ref name=":3">{{Cite journal|last=Kong|first=Andrew|last2=Van der Vliet|first2=Andrew|last3=Zadow|first3=Steven|date=2006-12-06|title=MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome|url=http://dx.doi.org/10.1007/s00330-006-0485-x|journal=European Radiology|volume=17|issue=7|pages=1772–1783|doi=10.1007/s00330-006-0485-x|issn=0938-7994}}</ref> | ||
* Thickened tendons | *Thickened tendons | ||
* Reduced echogenicity of tendons | * Reduced echogenicity of tendons | ||
* More heterogeneous echogenicity of tendons | *More heterogeneous echogenicity of tendons | ||
* Increased echogenicity of muscles as reduced muscle bulk and increased fat | *Increased echogenicity of muscles as reduced muscle bulk and increased fat | ||
* Partial tear are indicated by thinning of the tendon and partial thickness area free from echo | *Partial tear are indicated by thinning of the tendon and partial thickness area free from echo | ||
* Complete tear indicated by the full thickness of the tender being free from echo and a “bald” facet | *Complete tear indicated by the full thickness of the tender being free from echo and a “bald” facet | ||
* Deep to gluteus tendons insertions there may be cortical irregularities | *Deep to gluteus tendons insertions there may be cortical irregularities | ||
On Doppler Ultrasound can helpfully but uncommonly see increased vascularity<ref name=":3" /> | On Doppler Ultrasound can helpfully but uncommonly see increased vascularity<ref name=":3" /> | ||
| Line 32: | Line 56: | ||
<u>MRI</u><ref>{{Cite journal|last=Dadour|first=Joseph Rudy|last2=Gilbert|first2=Guillaume|last3=Lepage-Saucier|first3=Marianne|last4=Freire|first4=Véronique|last5=Bureau|first5=Nathalie J.|date=2021-04-29|title=Quantitative MRI in patients with gluteal tendinopathy and asymptomatic volunteers: initial results on T1- and T2*-mapping diagnostic accuracy and correlation with clinical assessment|url=http://dx.doi.org/10.1007/s00256-021-03781-0|journal=Skeletal Radiology|volume=50|issue=11|pages=2221–2231|doi=10.1007/s00256-021-03781-0|issn=0364-2348}}</ref> | <u>MRI</u><ref>{{Cite journal|last=Dadour|first=Joseph Rudy|last2=Gilbert|first2=Guillaume|last3=Lepage-Saucier|first3=Marianne|last4=Freire|first4=Véronique|last5=Bureau|first5=Nathalie J.|date=2021-04-29|title=Quantitative MRI in patients with gluteal tendinopathy and asymptomatic volunteers: initial results on T1- and T2*-mapping diagnostic accuracy and correlation with clinical assessment|url=http://dx.doi.org/10.1007/s00256-021-03781-0|journal=Skeletal Radiology|volume=50|issue=11|pages=2221–2231|doi=10.1007/s00256-021-03781-0|issn=0364-2348}}</ref> | ||
* Intensity of signal increased in T1w view within tendons of gluteus minimus and/or gluteus medius | *Intensity of signal increased in T1w view within tendons of gluteus minimus and/or gluteus medius | ||
* Hyperintensity in T2 view within tendon of gluteus minimus and/or gluteus medius | *Hyperintensity in T2 view within tendon of gluteus minimus and/or gluteus medius | ||
* Presence of fluid distension of the greater trochanteric bursa | *Presence of fluid distension of the greater trochanteric bursa | ||
* On coronal T1w view, fatty streaks or fatty infiltration of gluteus minimus and/or gluteus medius | *On coronal T1w view, fatty streaks or fatty infiltration of gluteus minimus and/or gluteus medius | ||
* Partial tear indicated by hyperintensity in T2 view within tendon of gluteus minimus and/or gluteus medius | *Partial tear indicated by hyperintensity in T2 view within tendon of gluteus minimus and/or gluteus medius | ||
* Partial tear can presents with or without tendon thinning | *Partial tear can presents with or without tendon thinning | ||
* Complete tear indicated by disruption of tendon of gluteus minimus and/or gluteus medius | *Complete tear indicated by disruption of tendon of gluteus minimus and/or gluteus medius | ||
* Osseous avulsion may or may not be present in a complete tear | *Osseous avulsion may or may not be present in a complete tear | ||
===Other Investigations=== | ===Other Investigations=== | ||
| Line 52: | Line 76: | ||
[[Lateral Hip Pain Differential Diagnoses|Lateral Hip Pain]] | [[Lateral Hip Pain Differential Diagnoses|Lateral Hip Pain]] | ||
==Treatment== | == Treatment== | ||
Gluteal tendinopathy for the majority is self limiting.<ref name=":4" /> It has been reported that more than 90% of people are responsive to conserverative treatment.<ref name=":4" /> Those who are not are considered refractory cases.<ref name=":4" /> | Gluteal tendinopathy for the majority is self limiting.<ref name=":4" /> It has been reported that more than 90% of people are responsive to conserverative treatment.<ref name=":4" /> Those who are not are considered refractory cases.<ref name=":4" /> | ||
| Line 69: | Line 93: | ||
[[Media:Gluteal tendinopathy va v12.png|LEAP trial]] | [[Media:Gluteal tendinopathy va v12.png|LEAP trial]] | ||
=== Surgery === | === Surgery=== | ||
Gluteal tendon reconstruction is experimental with no standardised techniques.<ref name=":0" /> If surgery is done it will involve a combination of some of the procedures listed: bursectomy, ITB release, trochanteric reduction osteotomy and gluteal tendon repair.<ref name=":4" /> | Gluteal tendon reconstruction is experimental with no standardised techniques.<ref name=":0" /> If surgery is done it will involve a combination of some of the procedures listed: bursectomy, ITB release, trochanteric reduction osteotomy and gluteal tendon repair.<ref name=":4" /> | ||
==Follow Up and Prognosis== | ==Follow Up and Prognosis== | ||
| Line 76: | Line 100: | ||
==Summary== | ==Summary== | ||
* Aetiology and pathophysiology for gluteal tendinopathy remains unclear | *Aetiology and pathophysiology for gluteal tendinopathy remains unclear | ||
* Prevalence is highest in women over 40 years | *Prevalence is highest in women over 40 years | ||
* Both athletes and sedentary individuals are affected | *Both athletes and sedentary individuals are affected | ||
* History of lateral hip pain | *History of lateral hip pain | ||
* Examination of lateral hip pain reproduced on FABER test and 30s single-leg stance test | *Examination of lateral hip pain reproduced on FABER test and 30s single-leg stance test | ||
* No set diagnostic criteria | *No set diagnostic criteria | ||
* Diagnosis is typically clinical | *Diagnosis is typically clinical | ||
* Imaging can be done with MRI being gold standard but ultrasound more clinically available | *Imaging can be done with MRI being gold standard but ultrasound more clinically available | ||
* No universally prescribed treatment protocol but LEAP protocol provides some promise | *No universally prescribed treatment protocol but LEAP protocol provides some promise | ||
* Conservative treatment effective in more than 90% of cases | *Conservative treatment effective in more than 90% of cases | ||
==Downloads== | ==Downloads== | ||
| Line 92: | Line 116: | ||
{{PDF|LEAP_Protocol.pdf|LEAP Protocol}} | {{PDF|LEAP_Protocol.pdf|LEAP Protocol}} | ||
== Links == | ==Links== | ||
[https://dralisongrimaldi.com/blog/how-physiotherapists-treat-gluteal-tendinopathy/ How physiotherapists treat gluteal tendinopathy by Dr Alison Grimaldi] | [https://dralisongrimaldi.com/blog/how-physiotherapists-treat-gluteal-tendinopathy/ How physiotherapists treat gluteal tendinopathy by Dr Alison Grimaldi] | ||
==References== | ==References== | ||
<references/> | <references /> | ||
{{Reliable sources|synonym1=Trochanteric+Bursitis|synonym2=Greater+Trochanteric+Pain+Syndrome}} | {{Reliable sources|synonym1=Trochanteric+Bursitis|synonym2=Greater+Trochanteric+Pain+Syndrome}} | ||
Revision as of 18:02, 11 April 2022
| |
| Gluteal Tendinopathy |
|---|
Greater trochanteric pain syndrome (GTPS) is an umbrella term encompassing different musculoskeletal entities that may contribute to chronic lateral hip pain. Tendinopathy of gluteus medius and/or gluteus minimus is the most common cause of GTPS and is generally simply referred to as gluteal tendinopathy. Other causes of GTPS are coxa saltans (snapping hip) with disorders of tensor fascia lata and/or the iliotibial band, and trochanteric bursitis. However, any inflamed or enlarged bursa seen (sub-gluteal minimus/medius) is invariably secondary to or co-exists with an underlying gluteal tendinopathy. Therefore the terms "trochanteric bursitis" and "trochanteritis" are generally regarded as misnomers.
Anatomy
In the "rotator cuff of the hip" there are six external rotators and three internal rotators.
- The external rotators are piriformis, gemellus superior and inferior, obturator internus, obturator externus, and quadratus femoris.
- The internal rotators are gluteus minimus, gluteus medius, and tensor fascia lata.
Gluteus medius is a large fan-shaped muscle that has its origin at the outer edge of the iliac crest running from the anterior superior iliac spine (ASIS) to the posterior superior iliac spine (PSIS). It has three equal portions: anterior, middle, and posterior. The anterior and middle portions assist with initiating hip abduction. The posterior portion is active in heel strike to full stance during gait to stabilise the hip. It inserts at the superoposterior and lateral facets of the greater trochanter.
Aetiology and Pathophysiology
Gluteal tendinopathy is caused by exposure to load that the tendon did not have adequate adaption or recovery time in order manage.[1][2] This could be due to a traumatic event (e.g. direct blow) or a frequent and repeated exposure to a load (e.g. jumping athlete).[2][1] Three continuous stages of disease have been described: normal to reactive tendinopathy to tendon dysrepair to degenerative tendinopathy.[1] This is explained in more detail in Tendinopathy. It is difficult because pain is not closely connected to progression of pathology.[2]
Epidemiology and Risk Factors
Common condition with prevalence highest in women over 40 years old.[1] One study reporting 23.5% of females and 8.5% of men between 50-79 years being affected in community-based population.[3] A rapid increase in intensity and/or frequency of on gluteal tendons puts individuals at risk.[2] Both athletes and sedentary individuals are affected.[1]
Clinical Features
History
Lateral hip pain over greater trochanter.[1] Onset typically slow but can occur following a traumatic event (fall, forceful sporting action).[1] Pain typically worsened with time and can be associated with a change in physical activity.[1] Pain can radiate around the trochanter and down the lateral thigh.[1] Associated symptom of stiffness of hip on standing or walking following sitting.[1] Sleep can be significantly disturbed as pain is typically worse at night time and pain makes it difficult for sleeping on side.[1] Pain can cause significant disability, particularly with single leg standing activities e.g. dressing, walking and going up stairs or hills.[1]
Examination
The patient is assessed during gait to evaluate for a Trendelenburg pattern.
The most important sign is pain on palpation of the greater trochanter. Absence of pain on palpation would indicate an alternate diagnosis.[1]
Lateral hip pain reproduced on 30s single-leg stance test was a sensitivity and specificity of 100% and 97.3% respectively for gluteal tendinopathy. The high utility of the test is only maintained if lateral displacement of the hip is avoided. The examiner may provide gentle fingertip support to steady the patient.[1]
The FABER test is useful in the differential diagnosis as limited range of movement is associated with hip joint pathology but not gluteal tendinopathy.[1]
The Ober's test has been shown to lack diagnostic utility for gluteal tendinopathy.[1]
The resisted internal rotation test had a sensitivity of 92% and specificity of 85% for the detection of gluteus medius tears.
Investigations
MRI is gold standard as it can visualise changes associated with gluteal tendinopathy, such as tendon thickening and soft tissue oedema, the clearest.[1] MRI is also useful in excluding other causes of lateral hip pain.[1] However, MRI is expensive and not very accessible.[1] Consequently, ultrasound is typically used in clinical practice.[1] The accuracy of ultrasound in identifying gluteal tendinopathy is variable and dependent on operator experience and patient characteristics.[1] It is important to note that it is normal for radiological changes to be present in the asymptomatic population, thus, any findings need to be considered within the clinical context.[1]
Imaging Findings
Grey scale Ultrasound[4]
- Thickened tendons
- Reduced echogenicity of tendons
- More heterogeneous echogenicity of tendons
- Increased echogenicity of muscles as reduced muscle bulk and increased fat
- Partial tear are indicated by thinning of the tendon and partial thickness area free from echo
- Complete tear indicated by the full thickness of the tender being free from echo and a “bald” facet
- Deep to gluteus tendons insertions there may be cortical irregularities
On Doppler Ultrasound can helpfully but uncommonly see increased vascularity[4]
MRI[5]
- Intensity of signal increased in T1w view within tendons of gluteus minimus and/or gluteus medius
- Hyperintensity in T2 view within tendon of gluteus minimus and/or gluteus medius
- Presence of fluid distension of the greater trochanteric bursa
- On coronal T1w view, fatty streaks or fatty infiltration of gluteus minimus and/or gluteus medius
- Partial tear indicated by hyperintensity in T2 view within tendon of gluteus minimus and/or gluteus medius
- Partial tear can presents with or without tendon thinning
- Complete tear indicated by disruption of tendon of gluteus minimus and/or gluteus medius
- Osseous avulsion may or may not be present in a complete tear
Other Investigations
Other imaging techniques are currently being developed. These include ultrasound tissue characterisation and elastography.[1]
Diagnosis
No clear diagnostic criteria exists for gluteal tendinopathy.[6] Typically the diagnosis is made clinically.[6] The history most commonly involves lateral hip pain that is exacerbated by activity and lying on the affected side.[6] On examination, one would expect to find tenderness on palpation of the greater trochanter.[6] This is the most common clinical finding in gluteal tendinopathy.[6]
Hip osteoarthritis is a common differential diagnosis for lateral hip pain. Asking about difficulty in manipulating shoes and socks is a useful way to differentiate the conditions.[7] A paper published in the British Journal of Sports Medicine suggested that diagnostic criteria for gluteal tendinopathy should include the patient reporting to have no difficulty in manipulating socks and shoes.[7] This paper also suggested the diagnostic criteria to include lateral hip pain reproduced on the FABER test as the FABER test should not produce lateral hip pain in hip osteoarthritis.[7]
Differential Diagnosis
Treatment
Gluteal tendinopathy for the majority is self limiting.[6] It has been reported that more than 90% of people are responsive to conserverative treatment.[6] Those who are not are considered refractory cases.[6]
Conservative treatment can include physiotherapy, shockwave therapy, NSAIDs, corticosteroid injections (CSI) and PRP injections.[6] There are varying levels of evidence for each of these interventions. Evidence does not support the conservative treatment of deep transverse friction massage, therapeutic ultrasound and acupuncture.[6]
Physiotherapy that is based around eccentric exercises has been shown to be effective in other tendinopathies.[6] Therefore, eccentric exercise has promise in the treatment of gluteal tendinopathy.
Ultrasound can be used for needle guidance of CSI. The injectate is deposited directly on the bone and around the injections or into the tendon itself. However, no significant difference between ultrasound guided and blind injection outcomes have been found.[6] CSI may provide benefit in the short term but with a high recurrence rate and poorer results in the long term.
Given the paucity of treatments for chronic gluteal tendinopathy (>3 months) and transient amelioration effect of CSI, there is interest whether biologic products such as PRP may provide better long-term outcomes for this condition.[8] The use of PRP has been controversial, especially in tendinopathies given its slower onset of action to see its efficacy. Some tendons respond differently to PRP. Technician skills, type of condition being treated and type of PRP used are all variables that can affect its effectiveness.
There is no universally prescribed treatment protocol.[6] However, the LEAP protocol is shown to be promising when compared to no treatment and single corticosteroid injection. The LEAP protocol involves education on load management (e.g. avoiding lying on side of affected leg) and a specific exercise programme.[9] This study and its results can be found in the resources below.
Exercise
Leap Trial
Surgery
Gluteal tendon reconstruction is experimental with no standardised techniques.[8] If surgery is done it will involve a combination of some of the procedures listed: bursectomy, ITB release, trochanteric reduction osteotomy and gluteal tendon repair.[6]
Follow Up and Prognosis
Over 90% respond to conservative treatment but there are still large number of patients thar fail non-operative treatment with significant levels of dysfunction making important to find novel treatment strategies.
Summary
- Aetiology and pathophysiology for gluteal tendinopathy remains unclear
- Prevalence is highest in women over 40 years
- Both athletes and sedentary individuals are affected
- History of lateral hip pain
- Examination of lateral hip pain reproduced on FABER test and 30s single-leg stance test
- No set diagnostic criteria
- Diagnosis is typically clinical
- Imaging can be done with MRI being gold standard but ultrasound more clinically available
- No universally prescribed treatment protocol but LEAP protocol provides some promise
- Conservative treatment effective in more than 90% of cases
Downloads
Links
How physiotherapists treat gluteal tendinopathy by Dr Alison Grimaldi
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 Grimaldi, Alison; Mellor, Rebecca; Hodges, Paul; Bennell, Kim; Wajswelner, Henry; Vicenzino, Bill (2015-05-13). "Gluteal Tendinopathy: A Review of Mechanisms, Assessment and Management". Sports Medicine. 45 (8): 1107–1119. doi:10.1007/s40279-015-0336-5. ISSN 0112-1642.
- ↑ 2.0 2.1 2.2 2.3 Cook, J L; Purdam, C R (2008-09-23). "Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy". British Journal of Sports Medicine. 43 (6): 409–416. doi:10.1136/bjsm.2008.051193. ISSN 0306-3674.
- ↑ Segal, Neil A.; Torner, James; Xie, Hui; Felson, David; Curtis, Jeffrey R.; Nevitt, Michael (2006-11-01). "PR_092: Greater Trochanteric Pain Syndrome: Epidemiology and Associated Factors". Archives of Physical Medicine and Rehabilitation (in English). 87 (11): e20. doi:10.1016/j.apmr.2006.08.114. ISSN 0003-9993.
- ↑ 4.0 4.1 Kong, Andrew; Van der Vliet, Andrew; Zadow, Steven (2006-12-06). "MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome". European Radiology. 17 (7): 1772–1783. doi:10.1007/s00330-006-0485-x. ISSN 0938-7994.
- ↑ Dadour, Joseph Rudy; Gilbert, Guillaume; Lepage-Saucier, Marianne; Freire, Véronique; Bureau, Nathalie J. (2021-04-29). "Quantitative MRI in patients with gluteal tendinopathy and asymptomatic volunteers: initial results on T1- and T2*-mapping diagnostic accuracy and correlation with clinical assessment". Skeletal Radiology. 50 (11): 2221–2231. doi:10.1007/s00256-021-03781-0. ISSN 0364-2348.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 Reid, Diane (2016-03). "The management of greater trochanteric pain syndrome: A systematic literature review". Journal of Orthopaedics. 13 (1): 15–28. doi:10.1016/j.jor.2015.12.006. ISSN 0972-978X. Check date values in:
|date=(help) - ↑ 7.0 7.1 7.2 Fearon, Angela M; Scarvell, Jennie M; Neeman, Terry; Cook, Jill L; Cormick, Wes; Smith, Paul N (2013-07). "Greater trochanteric pain syndrome: defining the clinical syndrome". British Journal of Sports Medicine (in English). 47 (10): 649–653. doi:10.1136/bjsports-2012-091565. ISSN 0306-3674. Check date values in:
|date=(help) - ↑ 8.0 8.1 Koulischer, Simon; Callewier, Antoine; Zorman, David (June 2017). "Management of greater trochanteric pain syndrome : a systematic review". Acta Orthopaedica Belgica. 83 (2): 205–214. ISSN 0001-6462. PMID 30399983.
- ↑ Mellor, Rebecca; Bennell, Kim; Grimaldi, Alison; Nicolson, Philippa; Kasza, Jessica; Hodges, Paul; Wajswelner, Henry; Vicenzino, Bill (2018-05-02). "Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial". BMJ: k1662. doi:10.1136/bmj.k1662. ISSN 0959-8138.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,