Histamine: Difference between revisions
| Line 55: | Line 55: | ||
== Histamine Receptors == | == Histamine Receptors == | ||
The | Histamine exerts its effects primarily by binding to G protein-coupled histamine receptors, designated H<sub>1</sub> through H<sub>4</sub>. Histamine also activates ligand-gated chloride channels in the brain and intestinal epithelium. The table below is from [[wikipedia:Histamine|wikipedia]]. | ||
{| class="wikitable" | |||
|+Biological targets of histamine | |||
!G-protein coupled receptor | |||
!Location | |||
!Function | |||
|- | |||
|H1 receptor | |||
|• '''CNS''': Expressed on the dendrites of the output neurons of the histaminergic tuberomammillary nucleus, which projects to the dorsal raphe, locus coeruleus, and additional structures. | |||
• '''Periphery''': Smooth muscle, endothelium, sensory nerves | |||
|• '''CNS''': Sleep-wake cycle (promotes wakefulness), body temperature, nociception, endocrine homeostasis, regulates appetite, involved in cognition | |||
• '''Periphery''': Causes bronchoconstriction, bronchial smooth muscle contraction, urinary bladder contractions, vasodilation, promotes hypernociception (visceral hypersensitivity), involved in itch perception and urticaria. | |||
|- | |||
|H2 receptor | |||
|• '''CNS''': Dorsal striatum (caudate nucleus and putamen), cerebral cortex (external layers), hippocampal formation, dentate nucleus of the cerebellum | |||
• '''Periphery''': Located on parietal cells, vascular smooth muscle cells, neutrophils, mast cells, as well as on cells in the heart and uterus | |||
|• '''CNS''': Not established (note: most known H<sub>2</sub> receptor ligands are unable to cross the blood–brain barrier in sufficient concentrations to allow for neuropsychological and behavioral testing) | |||
• '''Periphery''': Primarily involved in vasodilation and stimulation of gastric acid secretion. Urinary bladder relaxation. Modulates gastrointestinal function. | |||
|- | |||
|H3 receptor | |||
|Located in the central nervous system and to a lesser extent peripheral nervous system tissue | |||
|Autoreceptor and heteroreceptor functions: decreased neurotransmitter release of histamine, acetylcholine, norepinephrine, serotonin. Modulates nociception, gastric acid secretion, and food intake. | |||
|- | |||
|H4 receptor | |||
|Located primarily on basophils and in the bone marrow. It is also expressed in the thymus, small intestine, spleen, and colon. | |||
|Plays a role in mast cell chemotaxis, itch perception, cytokine production and secretion, and visceral hypersensitivity. Other putative functions (e.g., inflammation, allergy, cognition, etc.) have not been fully characterized. | |||
|- | |||
!Ligand-gated ion channel | |||
!Location | |||
!Function | |||
|- | |||
|Histamine-gated chloride channel | |||
|Putatively: CNS (hypothalamus, thalamus) and intestinal epithelium | |||
|Brain: Produces fast inhibitory postsynaptic potentials | |||
Intestinal epithelium: chloride secretion (associated with secretory diarrhea) | |||
|} | |||
[[Category:Pharmacology]] | [[Category:Pharmacology]] | ||
Revision as of 09:27, 23 August 2021
Histamine, or 2-(4-imidazolyl)-ethylamine, a is biogenic amine. It is synthesised through the decarboxylation of the amino acid histidine primarily in mast cells.
Itch
Itch Clinical Effects
Itch is thought to be a significant aspect of nociception. It has many similarities to pain, but generates a different behavioural response. Pain elicits a withdrawal reflex, while itch elicits a scratch reflex.
Following a stimulus resulting in itch, the individual experience itch at the site which persists briefly after the stimulus is removed. Following this there is a poorly localised area around the stimulus site, which when exposed to gentle touch, elicits intense itch. This is called alloknesis, and is analogous to allodynia.
There are four types of itch
- Pruritoceptive itch, transmitted by C fibres e.g. with inflammation or skin dryness
- Neuropathic itch, the archetypal disease being post-herpetic neuropathic pain. There is a loss of peripheral sensory neurons, which may lead to hyperactivity in the central itch-specific neurons or possibly disinhibit second order neurons.
- Neurogenic itch, occurs without any neural pathology. For example cholestatic itch (through opioid peptides synthesised by the liver), and exogenous opioid agonism on mu receptors.
- Psychogenic itch, such as in delusional parasitosis.
Itch Neurophysiology
Itch is transmitted by a dedicated subclass of C fibres, distinct from the polymodal C fibres involved in pain transmission. These so-called "itch neurons" have extensive terminal branching, slow conduction velocities, and a long lasting response to histamine. Itch neurons are not sensitive to mechanical stimuli.
There are no specific itch receptors on peripheral nerve endings in the skin, unlike what we see with pain. It is thought that there may be such receptors in second order neurons.
In the cerebral cortex, with itch PET imaging has shown co-activation of the anterior cingulate cortex, supplementary motor area, and inferior parietal lobe. The activation pattern is similar to that of pain, but without activation of the thalamic and somatosensory cortex.
The reason why rubbing inhibits the sensation of itch is because this stimulates myelinated A fibre low threshold mechanoreceptors. Scratching also inhibits itch though the stimulation of nociceptors.
Clinical Relevance
Pruritis is seen in many medical conditions such as CKD, lymphoma, HIV, post-herpetic neuralgia, multiple sclerosis, cholestasis, and certain dermatological conditions.
Itch is a common side effect of morphine. This is not an allergic reaction, but rather due to activation of mu receptors. Kappa and delta agonism does not evoke a similar response. Consequently, naltrexone an opioid receptor antagonist, reduces the itch from morphine, but histamine antagonists have no effect.
Histamine Effects
Histamine is a hydrophilic vasoactive amine. It is a potent vasodilator being involved in the acute inflammatory response and plays a key role in many allergic reactions. It is involved in gastric acid section. It also is involved in neuromodulation in the central nervous system.
Mast cells are recruited to sites of tissue injury, and are also resident in most tissues. They release proinflammatory mediators, including NGF upon activation.
Triple Response of Lewis
The "triple response of Lewis" is a cutaneous response that occurs from the firm stroking of the skin. The same response occurs with the intradermal injection of histamine.
- Red spot, appears within a few seconds caused by capillary vasodilation.
- Flare, develops slowly as a redness in the surrounding area due to arteriolar dilation mediated by axon reflex.
- Wheal, develops within 1-2 minutes caused by exudation of extracellular fluid from capillaries and venules.
Role in Pain
Histamine is a neurotransmitter in both the CNS and PNS.
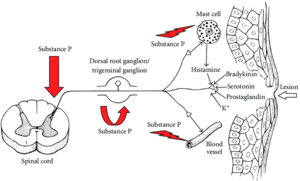
With chemical nociception and neurogenic inflammation, free nerve ending are stimulated by chemicals such as bradykinin and histamine. The nerve endings are stimulated to release substance P, which promotes vasodilation, enhancing inflammation and secondarily increases the release of the noxious chemicals and therefore secondarily enhance the stimulation of the nerve fibres.
In the epidermis it causes itching, and in the dermis it causes pain with or without itching.
In the superficial layers of the skin, the release of histamine from mast cells is a pruritogenic event through the bending of H1 receptors in the terminal membranes of a special subgroup of C-afferent fibres.
Histamine causes the release of prostaglandin E2 which sensitises pain receptors (see NSAIDs). It plays a role in acute inflammation related to mast cell degranulation, but it has an uncertain role in chronic inflammation. At low levels it may cause an itching sensation, and pain at higher levels.
Histamine Receptors
Histamine exerts its effects primarily by binding to G protein-coupled histamine receptors, designated H1 through H4. Histamine also activates ligand-gated chloride channels in the brain and intestinal epithelium. The table below is from wikipedia.
| G-protein coupled receptor | Location | Function |
|---|---|---|
| H1 receptor | • CNS: Expressed on the dendrites of the output neurons of the histaminergic tuberomammillary nucleus, which projects to the dorsal raphe, locus coeruleus, and additional structures.
• Periphery: Smooth muscle, endothelium, sensory nerves |
• CNS: Sleep-wake cycle (promotes wakefulness), body temperature, nociception, endocrine homeostasis, regulates appetite, involved in cognition
• Periphery: Causes bronchoconstriction, bronchial smooth muscle contraction, urinary bladder contractions, vasodilation, promotes hypernociception (visceral hypersensitivity), involved in itch perception and urticaria. |
| H2 receptor | • CNS: Dorsal striatum (caudate nucleus and putamen), cerebral cortex (external layers), hippocampal formation, dentate nucleus of the cerebellum
• Periphery: Located on parietal cells, vascular smooth muscle cells, neutrophils, mast cells, as well as on cells in the heart and uterus |
• CNS: Not established (note: most known H2 receptor ligands are unable to cross the blood–brain barrier in sufficient concentrations to allow for neuropsychological and behavioral testing)
• Periphery: Primarily involved in vasodilation and stimulation of gastric acid secretion. Urinary bladder relaxation. Modulates gastrointestinal function. |
| H3 receptor | Located in the central nervous system and to a lesser extent peripheral nervous system tissue | Autoreceptor and heteroreceptor functions: decreased neurotransmitter release of histamine, acetylcholine, norepinephrine, serotonin. Modulates nociception, gastric acid secretion, and food intake. |
| H4 receptor | Located primarily on basophils and in the bone marrow. It is also expressed in the thymus, small intestine, spleen, and colon. | Plays a role in mast cell chemotaxis, itch perception, cytokine production and secretion, and visceral hypersensitivity. Other putative functions (e.g., inflammation, allergy, cognition, etc.) have not been fully characterized. |
| Ligand-gated ion channel | Location | Function |
| Histamine-gated chloride channel | Putatively: CNS (hypothalamus, thalamus) and intestinal epithelium | Brain: Produces fast inhibitory postsynaptic potentials
Intestinal epithelium: chloride secretion (associated with secretory diarrhea) |
Resources
- See open access article on the role of histamine in neuropathic pain by Obara et al.[1]

