Lumbar Transforaminal Epidural Steroid Injection: Difference between revisions
(Created page with "{{Partial}}{{procedure |indication= |syringe= |needle= |steroid= |local= |volume= }} There are a variety of methods for epidural steroid injection for the treatment of lumbar...") |
|||
| Line 7: | Line 7: | ||
|volume= | |volume= | ||
}} | }} | ||
There are a variety of methods for epidural steroid injection for the treatment of lumbar radicular pain. The highest quality outcome data are weighted towards the transforaminal technique. Alternative options are interlaminar, and [[Caudal Epidural Steroid Injection|caudal]] injection. | There are a variety of methods for epidural steroid injection for the treatment of [[Lumbar Radicular Pain|lumbar radicular pain]]. The highest quality outcome data are weighted towards the transforaminal technique. Alternative options are interlaminar, and [[Caudal Epidural Steroid Injection|caudal]] injection. Transforaminal epidural injections should be done in accordance with the Spine Intervention Society guidelines under fluoroscopic guidance. CT guidance is an alternative method typically used by radiologists rather than Musculoskeletal physicians. | ||
==Anatomy== | ==Anatomy== | ||
| Line 16: | Line 16: | ||
There have been many proposed mechanisms for the effect of epidural steroid injections. They include anti-inflammatory effects, anti-nociceptive effects (blocking of C-fibre transmission<ref>Siddall PJ, Cousins MJ. Spinal pain mechanisms. Spine (Phila Pa 1976). 1997 Jan 1;22(1):98-104. doi: 10.1097/00007632-199701010-00016. PMID: 9122790.</ref>), suppression of immune response, mechanical debridement (washing away of inflammatory mediators), stopping the "pain-spasm" cycle, and placebo effect. | There have been many proposed mechanisms for the effect of epidural steroid injections. They include anti-inflammatory effects, anti-nociceptive effects (blocking of C-fibre transmission<ref>Siddall PJ, Cousins MJ. Spinal pain mechanisms. Spine (Phila Pa 1976). 1997 Jan 1;22(1):98-104. doi: 10.1097/00007632-199701010-00016. PMID: 9122790.</ref>), suppression of immune response, mechanical debridement (washing away of inflammatory mediators), stopping the "pain-spasm" cycle, and placebo effect. | ||
=== Radicular Pain === | |||
The primary indication for transforaminal epidural steroid injection is for [[Lumbar Radicular Pain|lower extremity radicular pain]] due to lumbar disc herniation in patients:<ref name=":0">Bogduk N. Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd Ed. San Francisco: ISIS; 2013</ref> | The primary indication for transforaminal epidural steroid injection is for [[Lumbar Radicular Pain|lower extremity radicular pain]] due to lumbar disc herniation in patients:<ref name=":0">Bogduk N. Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd Ed. San Francisco: ISIS; 2013</ref> | ||
| Line 26: | Line 27: | ||
Probably the most important efficacy study is that by Ghahreman and colleagues.<ref>Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010 Aug;11(8):1149-68. doi: 10.1111/j.1526-4637.2010.00908.x. PMID: 20704666.</ref> It was a randomised controlled study where they compared transforaminal steroid with a variety of other control groups. Transforaminal steroid with local anaesthetic resulted in a successful primary outcome 54% of the time and was more effective than the control groups. Success was defined as at least 50% relief one month post injection. | Probably the most important efficacy study is that by Ghahreman and colleagues.<ref>Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010 Aug;11(8):1149-68. doi: 10.1111/j.1526-4637.2010.00908.x. PMID: 20704666.</ref> It was a randomised controlled study where they compared transforaminal steroid with a variety of other control groups. Transforaminal steroid with local anaesthetic resulted in a successful primary outcome 54% of the time and was more effective than the control groups. Success was defined as at least 50% relief one month post injection. | ||
A 2013 systematic review looked at 6 RCTs, 5 pragmatic comparative trials, and 12 observational trials. They found that up to 70% achieve 50% or more greater pain relief, they reduce health care consumption, are surgery sparing, are cost effective, and can be durable with 25-40% having 12 months of relief.<ref>MacVicar J, King W, Landers MH, Bogduk N. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Med. 2013 Jan;14(1):14-28. doi: 10.1111/j.1526-4637.2012.01508.x. Epub 2012 Oct 30. PMID: 23110347.</ref> | A 2013 systematic review looked at 6 RCTs, 5 pragmatic comparative trials, and 12 observational trials. They found that up to 70% achieve 50% or more greater pain relief, they reduce health care consumption, are surgery sparing, are cost effective, and can be durable with 25-40% having 12 months of relief. The procedure is slightly more effective for acute than chronic pain. 69% of patients with acute pain had benefit, compared to 57% with chronic pain.<ref name=":1">MacVicar J, King W, Landers MH, Bogduk N. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Med. 2013 Jan;14(1):14-28. doi: 10.1111/j.1526-4637.2012.01508.x. Epub 2012 Oct 30. PMID: 23110347.</ref> | ||
=== Spinal Stenosis === | |||
Epidural steroid injection is less effective for spinal stenosis. For example in one 2004 study of mixed caudal/transforaminal patients only around one third having relief of greater than 2 months, one third having relief of less than 2 months, and one third having no relief. There was an overall small magnitude of change.<ref>Delport EG, Cucuzzella AR, Marley JK, Pruitt CM, Fisher JR. Treatment of lumbar spinal stenosis with epidural steroid injections: a retrospective outcome study. Arch Phys Med Rehabil. 2004 Mar;85(3):479-84. doi: 10.1016/s0003-9993(03)00472-6. PMID: 15031837.</ref> However a pivotal 2014 RCT showed that there was no difference for pain or disability at 6 weeks between the steroid-anaesthetic group and anaesthetic only group.<ref>Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD, Bauer Z, Bresnahan BW, Avins AL, Nedeljkovic SS, Nerenz DR, Standaert C, Kessler L, Akuthota V, Annaswamy T, Chen A, Diehn F, Firtch W, Gerges FJ, Gilligan C, Goldberg H, Kennedy DJ, Mandel S, Tyburski M, Sanders W, Sibell D, Smuck M, Wasan A, Won L, Jarvik JG. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014 Jul 3;371(1):11-21. doi: 10.1056/NEJMoa1313265. Erratum in: N Engl J Med. 2014 Jul 24;371(4):390. PMID: 24988555.</ref> | Epidural steroid injection is less effective for spinal stenosis. For example in one 2004 study of mixed caudal/transforaminal patients only around one third having relief of greater than 2 months, one third having relief of less than 2 months, and one third having no relief. There was an overall small magnitude of change.<ref>Delport EG, Cucuzzella AR, Marley JK, Pruitt CM, Fisher JR. Treatment of lumbar spinal stenosis with epidural steroid injections: a retrospective outcome study. Arch Phys Med Rehabil. 2004 Mar;85(3):479-84. doi: 10.1016/s0003-9993(03)00472-6. PMID: 15031837.</ref> However a pivotal 2014 RCT showed that there was no difference for pain or disability at 6 weeks between the steroid-anaesthetic group and anaesthetic only group.<ref>Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD, Bauer Z, Bresnahan BW, Avins AL, Nedeljkovic SS, Nerenz DR, Standaert C, Kessler L, Akuthota V, Annaswamy T, Chen A, Diehn F, Firtch W, Gerges FJ, Gilligan C, Goldberg H, Kennedy DJ, Mandel S, Tyburski M, Sanders W, Sibell D, Smuck M, Wasan A, Won L, Jarvik JG. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014 Jul 3;371(1):11-21. doi: 10.1056/NEJMoa1313265. Erratum in: N Engl J Med. 2014 Jul 24;371(4):390. PMID: 24988555.</ref> | ||
| Line 49: | Line 51: | ||
==Equipment== | ==Equipment== | ||
Most steroid preparations contain preservatives (polyethylene glycol and/or benzyl alcohol), however the clinical effect seems undetectable. All particular steroids have larger particles than RBCs, with betamethasone being the smallest. Dexamethasone is a solution with no particles and is the preferred agent used in New Zealand. | |||
=== Steroid Choice === | |||
Most steroid preparations contain preservatives (polyethylene glycol and/or benzyl alcohol), however the clinical effect seems undetectable. All particular steroids have larger particles than RBCs, with betamethasone being the smallest. Dexamethasone is a solution with no particles and is the preferred agent used in New Zealand. | |||
In one study comparing dexamethasone versus triamcinolone for transforaminal injection, no difference was found in efficacy between the groups at 2 weeks, 3 months, and 6 months in one RCT. However the dexamethasone group had slightly more people needing three injections to achieve the same outcomes, but most still only required 1 (~50%) or 2 injections (~30%) for symptomatic relief.<ref name=":2">Kennedy DJ, Plastaras C, Casey E, Visco CJ, Rittenberg JD, Conrad B, Sigler J, Dreyfuss P. Comparative effectiveness of lumbar transforaminal epidural steroid injections with particulate versus nonparticulate corticosteroids for lumbar radicular pain due to intervertebral disc herniation: a prospective, randomized, double-blind trial. Pain Med. 2014 Apr;15(4):548-55. doi: 10.1111/pme.12325. Epub 2014 Jan 2. PMID: 24393129.</ref> | |||
==Technique== | ==Technique== | ||
===Fluoroscopy Guided=== | ===Fluoroscopy Guided Subpedicular Approach=== | ||
'''Subpedicular | The '''Subpedicular approach''', also known as the "safe triangle" approach is the standard technique for L1-2 through to L5-S1 | ||
* Target visualisation | * Target visualisation | ||
| Line 64: | Line 70: | ||
** Check lateral to confirm needle placement just posterior to vertebral body, adjacent to the caudal border of the pedicle above the target nerve. | ** Check lateral to confirm needle placement just posterior to vertebral body, adjacent to the caudal border of the pedicle above the target nerve. | ||
* Injection | * Injection | ||
** Inject contrast under live fluoroscopy, using digital subtraction if available. | ** '''Contrast''': Inject contrast under live fluoroscopy, using digital subtraction if available. | ||
** Watch for intravascular or intrathecal flow. Abort the procedure if intra-arterial or intrathecal flow seen. | ** Watch for intravascular or intrathecal flow. Abort the procedure if intra-arterial or intrathecal flow seen. | ||
** If flow is suboptimal then adjust the needle position. | ** If flow is suboptimal then adjust the needle position. | ||
** Following contrast inject local anaesthetic | ** '''Local Anaesthetic:''' Following contrast injection, inject a test dose local anaesthetic (e.g. 1mL of 2% preservative free lidocaine) | ||
** '''Steroid:''' If there is no central or contralateral neurologic change over the next 1-2 minutes steroid can then be injected. In New Zealand it is typically dexamethasone 10mg in 1mL. | |||
** A total volume of 3mL will cover both the superior and inferior intervertebral discs of the corresponding level of injection 88% of the time. | |||
=== Fluoroscopy Guided Retroneural or Infraneural Approach === | |||
'''Retroneural or infraneural''' (triangle of Kambin) approaches can be used in the event that anatomical constraints prevent the subpedicular approach, or when it is thought that it will be more likely to deliver the steroid to the target nerve at the interface with the compressive lesion.<ref name=":3">Murthy NS, Geske JR, Shelerud RA, Wald JT, Diehn FE, Thielen KR, Kaufmann TJ, Morris JM, Lehman VT, Amrami KK, Carter RE, Maus TP. The effectiveness of repeat lumbar transforaminal epidural steroid injections. Pain Med. 2014 Oct;15(10):1686-94. doi: 10.1111/pme.12497. Epub 2014 Jul 7. PMID: 25039323.</ref> | |||
=== Fluoroscopically Guided S1 Transforaminal Approach === | |||
'''S1 transforaminal injection''' is used for S1 radicular pain, most commonly due to L5-S1 paracentral disc herniation. It requires placing the needle through the posterior S1 foramen onto the pedicle of S1. | '''S1 transforaminal injection''' is used for S1 radicular pain, most commonly due to L5-S1 paracentral disc herniation. It requires placing the needle through the posterior S1 foramen onto the pedicle of S1. | ||
| Line 91: | Line 103: | ||
==Aftercare== | ==Aftercare== | ||
The injection | The majority of patients require only a single injection. One review found that of the patients who achieved ≥50% pain relief, 94% required one injection, and 4% required two injections to achieve this level of relief.<ref name=":1" /> | ||
One study found that 22.4% of patients had repeat injections within a year either in the hopes of achieving greater relief or for recovery of lost benefit. <ref name=":2" />Another study reported 42% having repeat injections within 6 months.<ref name=":3" /> | |||
In the event of an incomplete response at 2 weeks post-injection, one can consider a repeat injection.<ref name=":3" /> | |||
==Videos== | ==Videos== | ||
Revision as of 18:58, 3 January 2022
| Lumbar Transforaminal Epidural Steroid Injection | |
|---|---|
| Indication | |
There are a variety of methods for epidural steroid injection for the treatment of lumbar radicular pain. The highest quality outcome data are weighted towards the transforaminal technique. Alternative options are interlaminar, and caudal injection. Transforaminal epidural injections should be done in accordance with the Spine Intervention Society guidelines under fluoroscopic guidance. CT guidance is an alternative method typically used by radiologists rather than Musculoskeletal physicians.
Anatomy
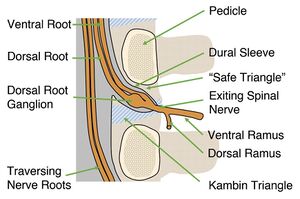
The safe triangle contains epidural fat. The epidural space is contained within the dural sleeve.
Indications and Efficacy
There have been many proposed mechanisms for the effect of epidural steroid injections. They include anti-inflammatory effects, anti-nociceptive effects (blocking of C-fibre transmission[1]), suppression of immune response, mechanical debridement (washing away of inflammatory mediators), stopping the "pain-spasm" cycle, and placebo effect.
Radicular Pain
The primary indication for transforaminal epidural steroid injection is for lower extremity radicular pain due to lumbar disc herniation in patients:[2]
- who require pain relief
- who have had a failed response to non-surgical intervention or non-surgical interventions aren't indicated
- whose pain likely has an inflammatory basis.
- whose symptoms are consistent with lumbar or sacral radicular pain and may or may not have radiculopathy.
- who have imaging findings that support the diagnosis of radicular pain
Probably the most important efficacy study is that by Ghahreman and colleagues.[3] It was a randomised controlled study where they compared transforaminal steroid with a variety of other control groups. Transforaminal steroid with local anaesthetic resulted in a successful primary outcome 54% of the time and was more effective than the control groups. Success was defined as at least 50% relief one month post injection.
A 2013 systematic review looked at 6 RCTs, 5 pragmatic comparative trials, and 12 observational trials. They found that up to 70% achieve 50% or more greater pain relief, they reduce health care consumption, are surgery sparing, are cost effective, and can be durable with 25-40% having 12 months of relief. The procedure is slightly more effective for acute than chronic pain. 69% of patients with acute pain had benefit, compared to 57% with chronic pain.[4]
Spinal Stenosis
Epidural steroid injection is less effective for spinal stenosis. For example in one 2004 study of mixed caudal/transforaminal patients only around one third having relief of greater than 2 months, one third having relief of less than 2 months, and one third having no relief. There was an overall small magnitude of change.[5] However a pivotal 2014 RCT showed that there was no difference for pain or disability at 6 weeks between the steroid-anaesthetic group and anaesthetic only group.[6]
Contraindications
Contraindications as outlined by the SIS guidelines are:[2]
- Absolute contraindications
- Informed consent not possible
- Not possible to use contrast medium
- Untreated local infection
- Patient non-cooperation despite consent.
- Pregnancy due to fluoroscopic use
- Relative contraindications
- Coagulopathy
- Anatomical abnormalities precluding safe intervention
- Systemic infection
- Significant cardiorespiratory compromise
- Immunosuppression
Pre-procedural Evaluation
Equipment
Steroid Choice
Most steroid preparations contain preservatives (polyethylene glycol and/or benzyl alcohol), however the clinical effect seems undetectable. All particular steroids have larger particles than RBCs, with betamethasone being the smallest. Dexamethasone is a solution with no particles and is the preferred agent used in New Zealand.
In one study comparing dexamethasone versus triamcinolone for transforaminal injection, no difference was found in efficacy between the groups at 2 weeks, 3 months, and 6 months in one RCT. However the dexamethasone group had slightly more people needing three injections to achieve the same outcomes, but most still only required 1 (~50%) or 2 injections (~30%) for symptomatic relief.[7]
Technique
Fluoroscopy Guided Subpedicular Approach
The Subpedicular approach, also known as the "safe triangle" approach is the standard technique for L1-2 through to L5-S1
- Target visualisation
- AP view through L4-5 disc space. Target position under pedicle identified just below 6 o' clock. However the AP view does not offer an unobstructed needle path
- Ipsilateral oblique (~25 degrees, exact amount depends on patient anatomy and level). Unobstructed needle path is visualised.
- Needle placement
- The needle insertion is marked In the ipsilateral oblique view, under the pedicle. Needle placement is down the beam approaching the target.
- Check AP to confirm needle placement at or just lateral to the 6 o clock pedicle position.
- Check lateral to confirm needle placement just posterior to vertebral body, adjacent to the caudal border of the pedicle above the target nerve.
- Injection
- Contrast: Inject contrast under live fluoroscopy, using digital subtraction if available.
- Watch for intravascular or intrathecal flow. Abort the procedure if intra-arterial or intrathecal flow seen.
- If flow is suboptimal then adjust the needle position.
- Local Anaesthetic: Following contrast injection, inject a test dose local anaesthetic (e.g. 1mL of 2% preservative free lidocaine)
- Steroid: If there is no central or contralateral neurologic change over the next 1-2 minutes steroid can then be injected. In New Zealand it is typically dexamethasone 10mg in 1mL.
- A total volume of 3mL will cover both the superior and inferior intervertebral discs of the corresponding level of injection 88% of the time.
Fluoroscopy Guided Retroneural or Infraneural Approach
Retroneural or infraneural (triangle of Kambin) approaches can be used in the event that anatomical constraints prevent the subpedicular approach, or when it is thought that it will be more likely to deliver the steroid to the target nerve at the interface with the compressive lesion.[8]
Fluoroscopically Guided S1 Transforaminal Approach
S1 transforaminal injection is used for S1 radicular pain, most commonly due to L5-S1 paracentral disc herniation. It requires placing the needle through the posterior S1 foramen onto the pedicle of S1.
- Target visualisation
- AP view through L5-S1 disc space, with a cephalo-caudad tilt
- Slight ipsilateral oblique, superimposing the anterior and posterior S1 foramina.
- The target point lies on the caudal border of the S1 pedicle, just dorsal to the internal opening of the S1 anterior sacral foramen.
- Needle placement
- The needle insertion point is marked at the lateral margin of the posterior foramen.
- Advance the needle towards the dorsal surface of the sacrum at the lateral margin of the S1 posterior foramen
- When the needle hits the sacrum, it is readjusted in order to pass superiorly and slightly medially into the S1 posterior sacral foramen. The aim is to hit the middle of the caudal border of the anterior half of the S1 pedicle.
- The needle shouldn't go medial tot he middle of the caudal border of the pedicle.
- Injection
- Inject contrast under live fluoroscopy, using digital subtraction if available.
- Watch for intravascular or intrathecal flow. Intravascular uptake is more common here.
- After contrast inject local anaesthetic followed by steroid. 3mL will cover the L5-S1 disc 92% of the time.
Ultrasound Guided
A cadaver study found that ultrasound guided transforaminal injection was almost as accurate as fluoroscopic guidance,[9] however it is not ready for prime time.
Complications
Aftercare
The majority of patients require only a single injection. One review found that of the patients who achieved ≥50% pain relief, 94% required one injection, and 4% required two injections to achieve this level of relief.[4]
One study found that 22.4% of patients had repeat injections within a year either in the hopes of achieving greater relief or for recovery of lost benefit. [7]Another study reported 42% having repeat injections within 6 months.[8]
In the event of an incomplete response at 2 weeks post-injection, one can consider a repeat injection.[8]
Videos
See Also
External Links
References
- ↑ Siddall PJ, Cousins MJ. Spinal pain mechanisms. Spine (Phila Pa 1976). 1997 Jan 1;22(1):98-104. doi: 10.1097/00007632-199701010-00016. PMID: 9122790.
- ↑ 2.0 2.1 Bogduk N. Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd Ed. San Francisco: ISIS; 2013
- ↑ Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010 Aug;11(8):1149-68. doi: 10.1111/j.1526-4637.2010.00908.x. PMID: 20704666.
- ↑ 4.0 4.1 MacVicar J, King W, Landers MH, Bogduk N. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Med. 2013 Jan;14(1):14-28. doi: 10.1111/j.1526-4637.2012.01508.x. Epub 2012 Oct 30. PMID: 23110347.
- ↑ Delport EG, Cucuzzella AR, Marley JK, Pruitt CM, Fisher JR. Treatment of lumbar spinal stenosis with epidural steroid injections: a retrospective outcome study. Arch Phys Med Rehabil. 2004 Mar;85(3):479-84. doi: 10.1016/s0003-9993(03)00472-6. PMID: 15031837.
- ↑ Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD, Bauer Z, Bresnahan BW, Avins AL, Nedeljkovic SS, Nerenz DR, Standaert C, Kessler L, Akuthota V, Annaswamy T, Chen A, Diehn F, Firtch W, Gerges FJ, Gilligan C, Goldberg H, Kennedy DJ, Mandel S, Tyburski M, Sanders W, Sibell D, Smuck M, Wasan A, Won L, Jarvik JG. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014 Jul 3;371(1):11-21. doi: 10.1056/NEJMoa1313265. Erratum in: N Engl J Med. 2014 Jul 24;371(4):390. PMID: 24988555.
- ↑ 7.0 7.1 Kennedy DJ, Plastaras C, Casey E, Visco CJ, Rittenberg JD, Conrad B, Sigler J, Dreyfuss P. Comparative effectiveness of lumbar transforaminal epidural steroid injections with particulate versus nonparticulate corticosteroids for lumbar radicular pain due to intervertebral disc herniation: a prospective, randomized, double-blind trial. Pain Med. 2014 Apr;15(4):548-55. doi: 10.1111/pme.12325. Epub 2014 Jan 2. PMID: 24393129.
- ↑ 8.0 8.1 8.2 Murthy NS, Geske JR, Shelerud RA, Wald JT, Diehn FE, Thielen KR, Kaufmann TJ, Morris JM, Lehman VT, Amrami KK, Carter RE, Maus TP. The effectiveness of repeat lumbar transforaminal epidural steroid injections. Pain Med. 2014 Oct;15(10):1686-94. doi: 10.1111/pme.12497. Epub 2014 Jul 7. PMID: 25039323.
- ↑ Hashemi, Masoud et al. “Ultrasound-Guided Lumbar Transforaminal Epidural Injections; A Single Center Fluoroscopic Validation Study.” Bulletin of emergency and trauma vol. 7,3 (2019): 251-255. doi:10.29252/beat-070307
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,