Lumbar Zygapophysial Joint Pain: Difference between revisions
(Created page with "== Anatomy == The lumbar zygapophysial joints are true synovial joints. They have hyaline cartilage that overlies the subchondral bone, a synovial membrane, a fibrous joint ca...") |
mNo edit summary |
||
| Line 1: | Line 1: | ||
{{Partial}} | |||
== Anatomy == | == Anatomy == | ||
The lumbar zygapophysial joints are true synovial joints. They have hyaline cartilage that overlies the subchondral bone, a synovial membrane, a fibrous joint capsule, and a joint space (1-2mL). | The lumbar zygapophysial joints are true synovial joints. They have hyaline cartilage that overlies the subchondral bone, a synovial membrane, a fibrous joint capsule, and a joint space (1-2mL). | ||
| Line 36: | Line 38: | ||
== References == | == References == | ||
<references /> | |||
[[Category:Lumbar Spine Conditions]] | |||
Revision as of 16:39, 7 September 2021
Anatomy
The lumbar zygapophysial joints are true synovial joints. They have hyaline cartilage that overlies the subchondral bone, a synovial membrane, a fibrous joint capsule, and a joint space (1-2mL).
Histological studies have shown encapsulated and free nerve endings, and the presence of substance P and calcitonin gene-related peptide.
Pathology
The causative pathology of lumbar zygapophysial joint pain is unknown.[1] It is thought to occur through trauma and cumulative stress over a lifetime. Possible sources are the synovial villi, capsule, and meniscal or synovial entrapments.
It can be illustrative to compare with the cervical zygapophysial joints. In the cervical spine the joints face upwards and backwards, and therefore equally share the compressive load with the discs. Injuries are most likely to occur from weight bearing, and degenerative changes occur at all levels, most commonly at C3/4.
In the lumbar spine, the zygapophysial joints face posteriorly and laterally, and share little of the axial load. The joints resist axial rotation and anterior translation. Degenerative changes arise earlier, most commonly at L4/5.
Excessive compression or torsion can lead to microfracture and capsular avulsion of the zygapophysial joints. These post-traumatic structural changes have been shown in laboratory studies and postmortem pathoanatomic studies, but not in any antemortem studies.[2]
Epidemiology
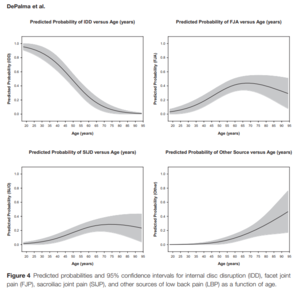
Lumbar zygapophysial joint pain is more common in older individuals. One example study found the prevalence to be 52% in the elderly, and 30% in adults.[4] On the whole, studies have reported prevalence rates of around 30%.[5] This compares to about 40% for disc pain, and 20% for sacroiliac joint pain.
There is no association with zygapophysial joint osteoarthritis.
Clinical Features
No reliable clinical features or imaging findings that are diagnostic
ZJ pain can cause back pain with referral into the lower limb Some cases of chronic low back pain can be relieved by anaesthetisation of the lumbar ZJ
- Like IDD, no clinical features that distinguish lumbar ZJ pain from other causes
- Often unilateral, but can be bilateral
- In a study by Mooney and Robertson[6], which demonstrated pain referral patterns of 5 normal and 15 abnormal volunteers (chronic LBP +/- sciatica) by injecting hypertonic saline:
- 2 patients – pain crossed the midline
- 3 patients – pain encompassed entire leg and foot
- Increased stimulus (i.e volume) = increased pain and increased radiation distally
- Localization of pain in the low back, buttock, and leg is a non-specific finding
- In all subjects, pain abolished by lignocaine
Diagnosis
The diagnostic criteria utilising controlled comparative diagnostic local anaesthetic blocks of the medial branches is the gold standard for diagnosis. This method has been shown to be durable over time with repeated testing at 1 year and 2 years.[7] A single block is not recommended due to the high false positive rate.[8]
References
- ↑ Bogduk. Low back pain In: Clinical and Radiological Anatomy of the Lumbar Spine. 5th Edition. Elsevier 2012
- ↑ Wade King and Nikolai Bogduk. Chronic Low Back Pain In: Bonica's Management of Pain. 2018
- ↑ DePalma MJ, Ketchum JM, Saullo T. What is the source of chronic low back pain and does age play a role? Pain Med. 2011 Feb;12(2):224-33. doi: 10.1111/j.1526-4637.2010.01045.x. Epub 2011 Jan 25. PMID: 21266006.
- ↑ Manchikanti L, Pampati V, Rivera J, Fellows B, Beyer C, Damron K. Role of facet joints in chronic low back pain in the elderly: a controlled comparative prevalence study. Pain Pract. 2001 Dec;1(4):332-7. doi: 10.1046/j.1533-2500.2001.01034.x. PMID: 17147574.
- ↑ DePalma MJ. Diagnostic Nihilism Toward Low Back Pain: What Once Was Accepted, Should No Longer Be. Pain Med. 2015 Aug;16(8):1453-4. doi: 10.1111/pme.12850. Epub 2015 Jul 27. PMID: 26218010.
- ↑ Mooney V, Robertson J. The facet syndrome. Clin Orthop Relat Res. 1976;115:149–156.
- ↑ Pampati S, Cash KA, Manchikanti L. Accuracy of diagnostic lumbar facet joint nerve blocks: a 2-year follow-up of 152 patients diagnosed with controlled diagnostic blocks. Pain Physician. 2009 Sep-Oct;12(5):855-66. PMID: 19787011.
- ↑ Manchikanti L, Kosanovic R, Pampati V, Cash KA, Soin A, Kaye AD, Hirsch JA. Low Back Pain and Diagnostic Lumbar Facet Joint Nerve Blocks: Assessment of Prevalence, False-Positive Rates, and a Philosophical Paradigm Shift from an Acute to a Chronic Pain Model. Pain Physician. 2020 Sep;23(5):519-530. PMID: 32967394.

