Nerve Conduction Studies: Difference between revisions
No edit summary |
No edit summary |
||
| Line 17: | Line 17: | ||
[[File:CMAP thenar muscles wrist and forearm.png|thumb|right|CMAPs recorded from the thenar muscles with stimulation of the left median nerve at the | [[File:CMAP thenar muscles wrist and forearm.png|thumb|right|CMAPs recorded from the thenar muscles with stimulation of the left median nerve at the | ||
wrist (upper potential at A1) and forearm (lower potential at A2). CMAPs, compound muscle action | wrist (upper potential at A1) and forearm (lower potential at A2). CMAPs, compound muscle action | ||
potentials.©<ref>Biller, José. Practical neurology. Philadelphia: Wolters Kluwer, 2017.</ref>]] | potentials.©<ref name="Biller">Biller, José. Practical neurology. Philadelphia: Wolters Kluwer, 2017.</ref>]] | ||
A-alpha fibres generate sensory nerve action potentials (SNAPs) and compound muscle action potentials (CMAPs). SNAPs and CMAPs are compound potentials representing summated electrical activity of individual nerve fibres with simultaneous activation of nerve stimulation. A-delta fibre electrical activity can be visualised through special techniques. | A-alpha fibres generate sensory nerve action potentials (SNAPs) and compound muscle action potentials (CMAPs). SNAPs and CMAPs are compound potentials representing summated electrical activity of individual nerve fibres with simultaneous activation of nerve stimulation. A-delta fibre electrical activity can be visualised through special techniques. | ||
| Line 28: | Line 28: | ||
===Temporal dispersion=== | ===Temporal dispersion=== | ||
[[File:SNAP median nerve wrist and forearm.png|thumb|right|Sensory nerve action potentials obtained while recording over the index finger with | [[File:SNAP median nerve wrist and forearm.png|thumb|right|Sensory nerve action potentials obtained while recording over the index finger with | ||
stimulation of the left median nerve at the wrist (upper response at A1) and forearm (lower response at A2).©<ref> | stimulation of the left median nerve at the wrist (upper response at A1) and forearm (lower response at A2).©<ref name="Biller"></ref>]] | ||
The largest and fastest conducting A-alpha fibres contribute to the earliest part of the compound evoked potentials, while slower conducting fibres contribute to the later parts. This is called temporal dispersion of electrical activities. The onset latency of a compound evoked potential is determined by the conduction speed of the fastest fibres. The duration of the evoked potential can be measured from the time it leaves the baseline to the time when it returns to the baseline. | The largest and fastest conducting A-alpha fibres contribute to the earliest part of the compound evoked potentials, while slower conducting fibres contribute to the later parts. This is called temporal dispersion of electrical activities. The onset latency of a compound evoked potential is determined by the conduction speed of the fastest fibres. The duration of the evoked potential can be measured from the time it leaves the baseline to the time when it returns to the baseline. | ||
Revision as of 20:44, 24 March 2021
Nerve conduction studies (NCS) allow the stimulation and recording of electrical activity from peripheral nerves. NCS is used to diagnose focal and generalised peripheral nerve disorders; aid in the differentiation between primary muscle and nerve disorders; classify peripheral nerve conduction abnormalities as being due to demyelination, axonal degeneration, or conduction block; and provide a prognosis on treatment effect and clinical course.
Anatomy and Normal Neurophysiology
Most peripheral nerves are mixed, comprising motor, sensory, and autonomic functions. There are certain primarily motor (e.g. anterior interosseous branch of the median nerve, posterior interosseous branch of the radial nerve) and primarily sensory fibres (e.g. sural nerve, peripheral peroneal nerve, superficial radial nerves) that allow neurophysiologic investigation.
Individual nerves are generally classified based on their diameters, conductivity, and myelin properties.
- A-alpha (or A-alpha beta): large myelinated fibers, 6 to 15 microns in diameter. The largest muscle afferent fibers are sometimes classified as 1a fibers.
- A-delta: small myelinated fibers, 3 to 5 microns in diameter.
- C fibers: unmyelinated fibers, 0.5 to 2 microns in diameter.
Most efferent motor fibres are A-alpha (large myelinated). A-alpha fibres also include sensory fibres providing touch, vibration, and position senses. Cold and fast pain sensations are mediated by A-delta fibres (small myelinated). Warm, itch, and slow pain sensations are mediated by C fibres (unmyelinated). C fibres also include efferent postganglionic sympathetic autonomic fibres.
Small-fibre neuropathy - where strength, vibration, and position are normal, but pain and temperature are abnormal - poses a problem with nerve conduction studies. This is because NCS can only evaluate the largest A-alpha fibres. In other words, NCS is normal in pure small-fibre neuropathies. A skin biopsy may be required for diagnosis in this case.
Compound action potentials
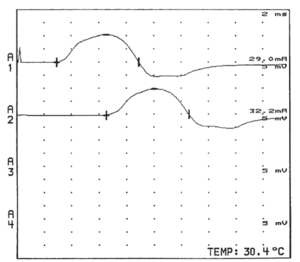
A-alpha fibres generate sensory nerve action potentials (SNAPs) and compound muscle action potentials (CMAPs). SNAPs and CMAPs are compound potentials representing summated electrical activity of individual nerve fibres with simultaneous activation of nerve stimulation. A-delta fibre electrical activity can be visualised through special techniques.
Myelinated fibre nerve conductivity is saltatory, via Ranvier (node-to-node) depolarisation. The speed of conduction is dependent on the nerve fibre diameter, with the largest fibres conducting the fastest. The relationship between diameter and velocity is roughly linear at a conversion factor of around 4.3m/s/micron in healthy individuals. 14 to 15 micron A-alpha fibres have a conduction velocity of around 65 to 70 m/s, and 6 to 7 micron A-alpha fibres at around 30 to 35 m/s
The SNAP peak-to-peak amplitude and area under the waveform represents the number of activated nerve fibres. The CMAP amplitude relates more to the number of activated muscle fibres rather than nerve fibres.
With an acute nerve lesion, before the onset of nerve regeneration, there is a loss of motor nerve fibres in parallel with the loss of activatable muscle fibres. Therefore CMAP amplitude is reduced. With chronic lesions, surviving motor units reinnervate the previously denervated muscle fibres through sprouting of collateral terminal motor nerve fibre branches. There are subsequently reduced numbers of motor fibres, each having increased motor unit territories and increased muscle fibre per motor units numbers. Therefore in this situation, CMAP amplitude is a poor estimate of motor nerve fibre number. The CMAP can have a normal or only mildly reduced amplitude. Motor unit number estimation (MUNE) and electromyography can be helpful in this situation.
Temporal dispersion
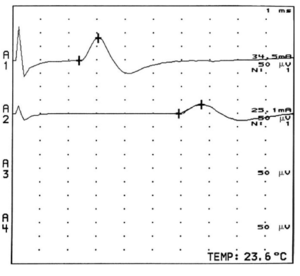
The largest and fastest conducting A-alpha fibres contribute to the earliest part of the compound evoked potentials, while slower conducting fibres contribute to the later parts. This is called temporal dispersion of electrical activities. The onset latency of a compound evoked potential is determined by the conduction speed of the fastest fibres. The duration of the evoked potential can be measured from the time it leaves the baseline to the time when it returns to the baseline.
The amplitude is greatest at the beginning, lessening as time goes on reflecting the differences in conduction speed of the different A-alpha fibres. So when the distance increases between the stimulating and recording electrodes, you get an increase in temporal dispersion, and a decrease in amplitude.
Temporal dispersion can be characterised as abnormal with an an excessive difference in slowing between individual motor axons within a nerve. This is generally due to altered or damaged myelin. There are different criteria defining abnormal temporal dispersion. For example the American Association of Neuromuscular and Electrodiagnostic Medicine define abnormal temporal dispersion as a 30 percent or more increase in CMAP duration between proximal and distal sites. Note that the relationship between increasing nerve length segment and temporal dispersion is roughly linear for motor conduction, but not for sensory conduction.
See Also
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


