Referred Pain: Difference between revisions
| Line 1: | Line 1: | ||
{{Partial}} | |||
Referred pain is pain perceived in a region innervated by nerves different from those that innervate the actual source of pain. Referred pain is probably the most common presentation of pain. | Referred pain is pain perceived in a region innervated by nerves different from those that innervate the actual source of pain. Referred pain is probably the most common presentation of pain. | ||
| Line 19: | Line 21: | ||
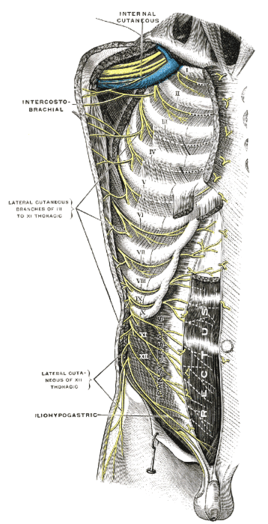
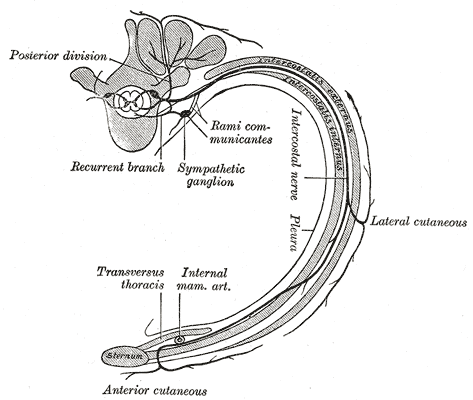
The simplest arrangement is the trunk with definable anatomical segments. Each segments has a rib, ligaments, muscles, (and skin). The limbs are a lot more complicated. Each intercostal nerve supplies the segment through which it runs. The nerves can be followed from the back around to the front. The upper thoracic nerves stay in their intercostal spaces and travel towards the sternum. The T6-L1 nerves pass across the costal margin, away from the sternum largely following the direction of the bones but not the costal cartilages, and into the abdominal region. They continue to supply the muscles and tissues in those bands. L2 and lower are distributed to the lower limbs. | The simplest arrangement is the trunk with definable anatomical segments. Each segments has a rib, ligaments, muscles, (and skin). The limbs are a lot more complicated. Each intercostal nerve supplies the segment through which it runs. The nerves can be followed from the back around to the front. The upper thoracic nerves stay in their intercostal spaces and travel towards the sternum. The T6-L1 nerves pass across the costal margin, away from the sternum largely following the direction of the bones but not the costal cartilages, and into the abdominal region. They continue to supply the muscles and tissues in those bands. L2 and lower are distributed to the lower limbs. | ||
<gallery mode=packed heights= | <gallery mode="packed" heights="350"> | ||
Intercostal nerves anterior view Gray.png|Intercostal nerves | File:Intercostal nerves anterior view Gray.png|Intercostal nerves. Note how the upper intercostal nerves angle towards the sternum, while the lower nerves follow the rib lines. | ||
Intercostal nerve Gray.png|The course and branches of a typical intercostal nerve | File:Intercostal nerve Gray.png|The course and branches of a typical intercostal nerve | ||
</gallery>For identification of a particular body segments, the upper segments can be identified based on the intercostal space. For a particular point on the chest, determine which rib lies above the point. For the abdomen there are no immediate cues. To determine the segment, trace the ribs from behind and see which rib points to that area. | </gallery>For identification of a particular body segments, the upper segments can be identified based on the intercostal space. For a particular point on the chest, determine which rib lies above the point. For the abdomen there are no immediate cues. To determine the segment, trace the ribs from behind and see which rib points to that area, ignoring the costal cartilages. For example, the 10th rib, if followed from behind and traced forward points towards the umbilicus. The epigastric region is T6, and L1 is just above the groin. These rules define the somatic segments of the trunk - the ribs, joints, muscles, and overlying skin. | ||
For referred pain in the limbs the body segments are more complex. | |||
== Visceral Referred Pain == | |||
{{Main|Visceral Pain}} | |||
When the viscera develop embryologically they start with a simple alimentary tract. They then obtain a nerve supply, with segments running from T1 to L2. This innervation is laid down before the development of individual organs. The alimentary tract starts to differentiate (stomach, caecum, etc) and becomes longer (small and large intestine). With this differentiation, the nerve supply is taken with the organs, rather than the organs differentiating and then the nerve supply finding that organ. This mapping can help clinically with pain stemming from different organs. | |||
The urinary tract is a separate system, but is innervated in a similar fashion with early laydown of nerves. And so similarly, the more cranial portions take more cranial innervation, and the most caudal portions take more caudal innervation. | |||
Diagnostically in the setting of visceral pain, the thought process should start with determining which body segment the patient is experiencing pain. The next step is considering which structures are innervated by those segments. The differential diagnosis may include muscles, joints, ribs, and visceral structures. | |||
A pain in a particular area does not necessarily correlate with a problem in an underlying organ. The organ refers pain to the particular area only if it shares the same nerve supply, regardless of its anatomical location. For example, the transverse colon may refer pain to the lower abdomen rather than the epigastrium. | |||
== Somatic Referred Pain == | |||
{{Main|Somatic Referred Pain}} | |||
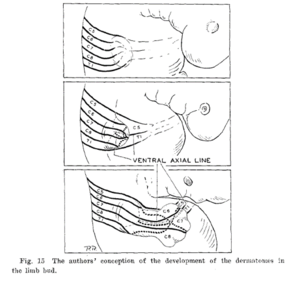
[[File:Keegan and Garrett dermatome embryology theory.png|thumb|There is a free course of outgrowing fibres through an already formed nerveless limb bud.]] | |||
In the limbs , embryologically, nerves are not present at all in early limb buds. At a later data plexuses form, and then the nerves grow more-or-less directly to their appropriate targets, with motor nerves being earlier than sensory nerves. The muscles form in bands and aggregate into individual muscles. | |||
In the skin, the segmental nerve supply runs from C4/C5 through to T1/2. The muscle nerve supply isn't as extensive as the skin, running from C5 through to T1. | |||
The topographical areas between skin and muscle supply are often different. For example with the muscles, T1 is in the hand unlike what is seen with skin. The muscle segments of the proximal limb contain C5-C8, the mid limb C6-C8, and the hand C8-T1. | |||
In the limbs, the segmentation of the deep innervation is distorted. The best guideline for determining which body part is supplied by which segment can be determined by knowing the [[Myotomes|segmental innervation of the muscles]] that act on particular joints or do particular movements. For example, if a patient has pain in the anterior arm, the diagnostic thought process should start with knowing that the body segments are C5-6, and then thinking through which tissues are supplied by C5-6. | |||
[[Category:Pain Types]] | [[Category:Pain Types]] | ||
[[Category:Neurophysiology]] | [[Category:Neurophysiology]] | ||
Revision as of 10:31, 21 August 2021
Referred pain is pain perceived in a region innervated by nerves different from those that innervate the actual source of pain. Referred pain is probably the most common presentation of pain.
Ascending Pathways
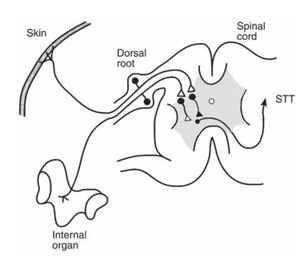
The pathways of stimuli coming from skin ascend up the spinal cord largely through the spinothalamic tract for noxious stimuli, and the posterior columns for tactile stimuli, and thence through to the thalamus. Different types of information is recorded by different pathways. This multiplicity endows skin stimuli with good localisation in the thalamus and the cerebral cortex. The ability to localise skin stimuli if the posterior columns are interrupted. There is good somatotopic organisation with a faithful continuation of representation of points in the skin to particular cells in the pathways.
In contrast, stimuli from deep structures such as bones, ligaments, joints, and muscles have a fairly restricted pathway largely through the spinothalamic tract, but also through collaterals into the reticular formation of the brainstem constituting the spinoreticulothalamic tract (SRTT). In this system there are a large number of neurons with several synapses and connections along the pathway. This system has poor somatotopic organisation.
In an evolutionary sense, there is no point in having an expensive highly localised sensory system for deep structures because unlike with the skin, there is nothing that the organism can do about pain in deep areas.
Convergence
In systems like the STT pathways that is relatively predominant in the innervation of deep structures, neurons are used economically. Two nerves in the periphery might converge on a single neuron. The axons of two of those neurons may converge on yet another single neuron, and so on. This pattern of converge is seen throughout the pathway: between primary afferent and cells in the spinal cord, between cells from the spinal card into the higher nuclei, and then onto the thalamus.
The frontal lobe therefore has no way of knowing which exact cell the stimuli originated from. In general the thalamus knows the location within plus or minus one spinal cord segment. In contrast to knowing a specific area of the big toe, it thinks the information is arising from around L5, but maybe L4 or S1.
Body Segments
Some authors state that referred pain occurs in dermatomes. This is neither an appropriate or accurate model for referred pain. There is no reliable or accurate relationship between the area of referred pain and the dermatome that seems to cover it. Therefore avoid describing referred pain in terms of dermatomal patterns. The term that is best applied is that of a body segment.
The simplest arrangement is the trunk with definable anatomical segments. Each segments has a rib, ligaments, muscles, (and skin). The limbs are a lot more complicated. Each intercostal nerve supplies the segment through which it runs. The nerves can be followed from the back around to the front. The upper thoracic nerves stay in their intercostal spaces and travel towards the sternum. The T6-L1 nerves pass across the costal margin, away from the sternum largely following the direction of the bones but not the costal cartilages, and into the abdominal region. They continue to supply the muscles and tissues in those bands. L2 and lower are distributed to the lower limbs.
For identification of a particular body segments, the upper segments can be identified based on the intercostal space. For a particular point on the chest, determine which rib lies above the point. For the abdomen there are no immediate cues. To determine the segment, trace the ribs from behind and see which rib points to that area, ignoring the costal cartilages. For example, the 10th rib, if followed from behind and traced forward points towards the umbilicus. The epigastric region is T6, and L1 is just above the groin. These rules define the somatic segments of the trunk - the ribs, joints, muscles, and overlying skin.
For referred pain in the limbs the body segments are more complex.
Visceral Referred Pain
- Main article: Visceral Pain
When the viscera develop embryologically they start with a simple alimentary tract. They then obtain a nerve supply, with segments running from T1 to L2. This innervation is laid down before the development of individual organs. The alimentary tract starts to differentiate (stomach, caecum, etc) and becomes longer (small and large intestine). With this differentiation, the nerve supply is taken with the organs, rather than the organs differentiating and then the nerve supply finding that organ. This mapping can help clinically with pain stemming from different organs.
The urinary tract is a separate system, but is innervated in a similar fashion with early laydown of nerves. And so similarly, the more cranial portions take more cranial innervation, and the most caudal portions take more caudal innervation.
Diagnostically in the setting of visceral pain, the thought process should start with determining which body segment the patient is experiencing pain. The next step is considering which structures are innervated by those segments. The differential diagnosis may include muscles, joints, ribs, and visceral structures.
A pain in a particular area does not necessarily correlate with a problem in an underlying organ. The organ refers pain to the particular area only if it shares the same nerve supply, regardless of its anatomical location. For example, the transverse colon may refer pain to the lower abdomen rather than the epigastrium.
Somatic Referred Pain
- Main article: Somatic Referred Pain
In the limbs , embryologically, nerves are not present at all in early limb buds. At a later data plexuses form, and then the nerves grow more-or-less directly to their appropriate targets, with motor nerves being earlier than sensory nerves. The muscles form in bands and aggregate into individual muscles.
In the skin, the segmental nerve supply runs from C4/C5 through to T1/2. The muscle nerve supply isn't as extensive as the skin, running from C5 through to T1.
The topographical areas between skin and muscle supply are often different. For example with the muscles, T1 is in the hand unlike what is seen with skin. The muscle segments of the proximal limb contain C5-C8, the mid limb C6-C8, and the hand C8-T1.
In the limbs, the segmentation of the deep innervation is distorted. The best guideline for determining which body part is supplied by which segment can be determined by knowing the segmental innervation of the muscles that act on particular joints or do particular movements. For example, if a patient has pain in the anterior arm, the diagnostic thought process should start with knowing that the body segments are C5-6, and then thinking through which tissues are supplied by C5-6.