Sacroiliac Joint Injection: Difference between revisions
No edit summary |
No edit summary |
||
| Line 26: | Line 26: | ||
==Technique== | ==Technique== | ||
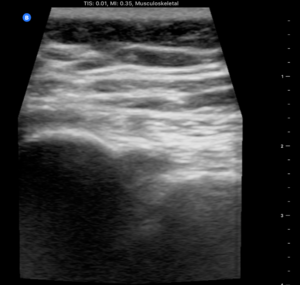
[[File:Sacroiliac joint left ultrasound.png|thumb|right|Left sacroiliac joint on ultrasound imaging, with the ilium on the left, and sacrum on the right]] | |||
[[File:Sacroiliac joint ultrasound cineloop.mp4|thumb|right|Locating the left sacroiliac joint. Moving caudally on the transverse plane from the lower lumbar spine to S2, then laterally to find the SIJ]] | |||
===Ultrasound Guided=== | ===Ultrasound Guided=== | ||
USS has been shown to have up to 90% success rate [Klauser et al] and even if not intraarticular then USS ensures peri-articular injection which is believed to be effective [Hartung et al] | USS has been shown to have up to 90% success rate [Klauser et al] and even if not intraarticular then USS ensures peri-articular injection which is believed to be effective [Hartung et al] | ||
Revision as of 08:21, 5 August 2020
| Sacroiliac Joint Injection | |
|---|---|
| Indication | sacroiliitis / ankylosing spondylitis, SIJ arthritis, SIJ dysfunction |
| Needle | 21gauge 70mm needle |
| Volume | The joint can take up to 2mL |
Background
SI joint has been shown to be a source of pain in 10-27% of suspected cases of chronic low back pain.
Anatomy
- Main article: Sacroiliac Joint Anatomy
The sacroiliac joint is around 1-2mm wide and is formed within S1, S2, and S3. The concave sacral surface joins with the convex ilium surface. The joint has an interlocking mechanism due to an irregular sacral surface. The capsule is often indistinguishable from the surrounding ligaments. The strongest ligament is the interosseous ligament. Other ligaments are the anterior and posterior sacroiliac ligaments, the sacrotuberous ligament which attaches to the coccygeal vertebrae and the ischial tuberosity, and the sacrospinous ligament which joins the ischial spine to the sacrum and coccyx. The anterior joint is thought to be innervated by the ventral rami of L4 and L5, and the posterior joint by the lateral branches of the posterior rami of L5-S4. The superior gluteal nerve contributes.
Indications
Diagnostic block for sacroiliitis / ankylosing spondylitis, SIJ arthritis, SIJ dysfunction, gout, rheumatoid arthritis, psoriasis, congenital deformity
Contraindications
Relative contraindications Bleeding diatheses, fracture, malignancy
Technique
Ultrasound Guided
USS has been shown to have up to 90% success rate [Klauser et al] and even if not intraarticular then USS ensures peri-articular injection which is believed to be effective [Hartung et al]
Landmarks: Patient in prone position. Bony landmarks of PSIS, spinous process L5.
USS landmarks: probe in transverse/axial view from L5, down to the sacral median crest. Probe then goes lateral over the sacrum until the PSIS is visible. The notch in between represents the joint in an axial view. The dorsal SIJ ligaments should be visible connecting the sacrum to the ilium.
Mark out the probe position with permanent marker.
Wipe down area, sterile field: skin prep, sterile jelly, sterile probe.
Needle placement: 1. Medial to lateral approach: place probe in position then needle enters skin in midline - approx 2cm from the heel of the probe and has a shallow trajectory towards probe. Needle tip will appear in joint when under the middle of the proble. 2. Caudal to cranial approach: The other option is to enter the needle caudally to the marker on the probe and aim cranially and laterally (15deg) until needle tip enters joint in the midline of the probe. The ultrasound probe placement for this approach is shown in the attached video.
Local anaesthetic: 27gauge needle USS guidance around and on top of the dorsal ligaments. Corticosteroid: 21gauge 70mm needle into joint and inject. Note the tactile sensation of pushing through leather then the release once in joint. Joint can take up to 2mm of steroid then will feel resistance.
Landmark Guided
This is not recommended. You can inject the dorsal sacroiliac ligaments but not the joint itself without ultrasound or fluoroscopic guidance. Because of the obliquity of the three dimensional anatomy blind injection is often unsuccessful [Hartung et al]
Complications
Infection - risk 1:10,000. Fatty atrophy. Skin depigmentation. Risks mitigated if sterile field and steroid not injected subcutaneously.
Aftercare
Post procedure: dressings, icepack, education, exercises, pain diary.
Videos
See Also
External Links
References
Hartung W, Ross CJ, Straub R, et al.: Ultrasound-guided sacroiliac joint injection in patients with established sacroiliitis: Precise IA injection verified by MRI scanning does not predict clinical outcome. Rheumatology (Oxford, England) 2010; 49: 1479–82
Klauser A, De Zordo T, Feuchtner G, et al.: Feasibility of ultrasound-guided sacroiliac joint injection considering sonoanatomic landmarks at two different levels in cadavers and patients. Arthritis Rheum 2008; 59: 1618–24