Sacroiliac Joint Pain
The sacroiliac joint is a common source of chronic low back pain. Pain generators are the joint itself, and the surrounding ligaments and muscles. There may be multiple factors coming from the bones, ligaments, muscles, motor control, and alignment.
Anatomy
- Main article: Sacroiliac Joint Anatomy
The sacroiliac joint is a diarthrodial synovial joint, and only the anterior aspect is a true synovial joint. The posterior aspect is a syndesmosis that consists of the gluteus medius, gluteus minimus, sacroiliac ligaments, and piriformis. [1] The anterior joint is thought to be innervated by the ventral rami of L4 and L5, and the posterior joint by the lateral branches of the posterior rami of L5-S4. The superior gluteal nerve contributes.
Epidemiology
The sacroiliac joint accounts for around 16% to 30% of causes of chronic low back pain. Some of the prevalence rates in diagnostic block research are 22.6% (Bernard 1987), 30% (Schwarzer 1995), 18.5% (Maigne 1996), 27% (Irwin 2007), 14.5% (Sembrano 2009).[2]
There are three primary groups of patients with sacroiliac joint pain and dysfunction. It occurs post lumbar fusion, in trauma, and in the peripartum. Pain can occur in all age groups from the very young to very old.
In symptomatic post-lumbar fusion patients, the sacroiliac joint is the source of pain about 30-40% of the time. Some of the prevalence rates in this context are 32% (Katz 2003), 35% (Maigne 2005), 43% (DePalma 2001), and 40% (Liliang 2011).[2]
Pathophysiology
- Post-lumbar fusion
Sacroiliac joint pain is almost akin to the idea of adjacent segment degeneration. In the event of L5-S1 fusion, there is 52% added motion on the sacroiliac joint. With L4-S1 fusion there is 168% added motion on the sacroiliac joint. Meanwhile if you fuse the sacroiliac joint, there is only 2-4% added motion on L4 and L5, and 5% added stress on the hip.[3]
Clinical Assessment
Pelvic Malalignment
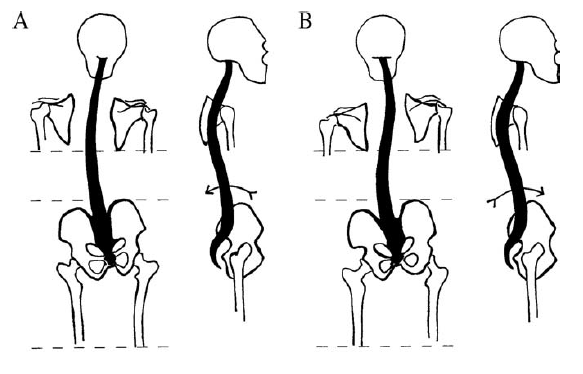
Timgren et al assessed pelvic asymmetry in neurologic patients with symptoms that weren't explained by a neurological diagnosis. They found pelvic asymmetry in 87%. Reestablishment and maintenance of symmetry correlated with improvement in pain and function. An average of 3.7 appointments was needed. They found the following patterns. [4]
| Innominate | A. Posterior rotation | B. Anterior Rotation |
|---|---|---|
| Iliac Crest | Elevated ↑ | Elevated ↑ |
| ASIS | Elevated ↑ | Depressed ↓ |
| PSIS | Depressed ↓ | Elevated ↑ |
| scapula | Depressed ↓ | Elevated ↑ |
| leg | Longer ↑ | Shorter ↓ |
| 10-15mm lift | Increased crest difference ↑ | Reduced crest difference ↓ |
| Spinal curvature | C type scoliosis | S type scoliosis |
| C0-C1 function | Symmetric rotation in flexion | Restricted rotation in flexion |
All changes are in reference the ipsilateral side.
Rising of the crest upon anterior SI rotation is paradoxical, and its explanation cannot be reduced to a two-dimensional model.
Schamberger’s rule of the five Ls, which relates to the side of the anteriorly rotated innominate: “Leg Lengthens Lying, Landmarks Lower” (supine vs long sitting) [5]
Treatment
Manual Therapy
Alignment can be reacquired through various means such as muscle energy techniques, and mobilisation with movement.
Mulligan Techniques
- Anterior Innominate Rotation
The most common malalignment is anterior rotation. This can usually be easily corrected with a mobilisation with movement technique called anterior innominate extension in lying mobilisation with movement. The sacrum is stabilised, the innominate is rotated and glided posteriorly, while the patient extends in lying. Ensure mobilisation is a combination of glide +/- rotation of the innominate with opposing forces on the sacrum. This technique often corrects posterior rotation, too.
- Mulligan Videos
Muscle Energy Techniques
Pelvic asymmetries can also be corrected with muscle energy techniques.
- Anterior Innominate Rotation
The technique can be visualised via the image below where the origin and insertion of the hamstrings are reversed to pull and rotate the innominate. Ensure to lean cranially, and allow some abduction of the ipsilateral hip. Stabilise the contralateral ASIS. Reach the end range of hip flexion and complete a muscle energy technique. The patient can treat themselves by grasping under their knees and resisting thigh extension, alternating on both sides. This again produces a correctional rotational force on the pelvis.
HVLA techniques
High-velocity and low-amplitude thrust technique can be applied through the ankle on the side of the dysfunctional SI joint
Precision Treatment
- Main article: Sacroiliac Joint Precision Treatment
The sacroiliac joint can treated with radiofrequency neurotomy after a confirmatory single or dual diagnostic block. Cooled radiofrequency neurotomy has an evidence base, while traditional radiofrequency does not.
Article Downloads
References
- ↑ Vanelderen et al.. 13. Sacroiliac joint pain. Pain practice : the official journal of World Institute of Pain 2010. 10:470-8. PMID: 20667026. DOI.
- ↑ 2.0 2.1 DePalma et al.. What is the source of chronic low back pain and does age play a role?. Pain medicine (Malden, Mass.) 2011. 12:224-33. PMID: 21266006. DOI.
- ↑ Ivanov et al.. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine 2009. 34:E162-9. PMID: 19247155. DOI.
- ↑ Timgren & Soinila. Reversible pelvic asymmetry: an overlooked syndrome manifesting as scoliosis, apparent leg-length difference, and neurologic symptoms. Journal of manipulative and physiological therapeutics 2006. 29:561-5. PMID: 16949945. DOI.
- ↑ Wolf Schamberger. The Malalignment Syndrome 2nd Edition. Churchill Livingstone. 2012
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,