Superior Cluneal Nerve Entrapment: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
{{stub}} | {{stub}} | ||
==Anatomy== | Some authors posit that cluneal nerve entrapment is an under-diagnosed cause of chronic low back pain, and it can cause neuropathic type symptoms. | ||
==Anatomy and Pathophysiology== | |||
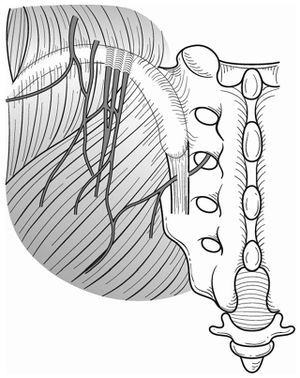
[[File:Superior and middle cluneal nerves.jpg|thumb|right|Superior and middle cluneal nerves with typical entrapment sites. Multiple branches of the superior cluneal nerves can be entrapped where they pierce the thoracolumbar fascia over the iliac crest. Middle cluneal nerve entrapment can occur where it passes under or through the long posterior sacroiliac ligament.{{#pmid:27004164|Aota}}]] | [[File:Superior and middle cluneal nerves.jpg|thumb|right|Superior and middle cluneal nerves with typical entrapment sites. Multiple branches of the superior cluneal nerves can be entrapped where they pierce the thoracolumbar fascia over the iliac crest. Middle cluneal nerve entrapment can occur where it passes under or through the long posterior sacroiliac ligament.{{#pmid:27004164|Aota}}]] | ||
Superior cluneal nerve (SCN) entrapment occurs where the nerve pierces the thoracolumbar attachment at the posterior iliac crest. The medial branch of the SCN consistently passes through an osteofibrous tunnel and can be spontaneously entrapped. | |||
The middle cluneal nerve (MCN) is comprised of the sensory branches of the S1 to S3 dorsal rami. It travels below the PSIS in an approximately horizontal route and supplies the skin overlying the posteromedial buttock. The S1 to S2 composition could explain why some patients may get leg symptoms. It can become trapped with passing underneith or through the long posterior sacroiliac ligament. MCN entrapment can be confused with sacroiliac joint pain. Even a positive sacroiliac joint block could still indicate LPSL pain or MCN entrapment if there is dorsal extravasation of the local anaesthetic. | |||
==Diagnosis== | |||
There is no gold standard diagnostic method. The diagnosis can be considered by tenderness over the iliac crest or LPSL causing provocation of symptoms. Pain relief following local anaesthetic injection can give further weight to the diagnosis. | |||
The SCN tender point is typically on the posterior iliac crest, approximately 70mm from the midline and 45mm from the PSIS. The MCN tender point is typically on the LPSL within 40mm caudal to the PSIS. | |||
==Treatment== | ==Treatment== | ||
===Injections=== | |||
Trigger point injections have been described. | |||
===Surgery=== | ===Surgery=== | ||
Reports have been published on | Reports have been published on SCN release and MCN release. Most reports are on SCN release. | ||
==References== | ==References== | ||
| Line 14: | Line 27: | ||
{{Reliable sources}} | {{Reliable sources}} | ||
[[Category:Lumbar Spine]] | |||
[[Category:Sacroiliac Joint]] | [[Category:Sacroiliac Joint]] | ||
[[Category:Stubs]] | [[Category:Stubs]] | ||
Revision as of 13:44, 7 September 2020
Some authors posit that cluneal nerve entrapment is an under-diagnosed cause of chronic low back pain, and it can cause neuropathic type symptoms.
Anatomy and Pathophysiology
Superior cluneal nerve (SCN) entrapment occurs where the nerve pierces the thoracolumbar attachment at the posterior iliac crest. The medial branch of the SCN consistently passes through an osteofibrous tunnel and can be spontaneously entrapped.
The middle cluneal nerve (MCN) is comprised of the sensory branches of the S1 to S3 dorsal rami. It travels below the PSIS in an approximately horizontal route and supplies the skin overlying the posteromedial buttock. The S1 to S2 composition could explain why some patients may get leg symptoms. It can become trapped with passing underneith or through the long posterior sacroiliac ligament. MCN entrapment can be confused with sacroiliac joint pain. Even a positive sacroiliac joint block could still indicate LPSL pain or MCN entrapment if there is dorsal extravasation of the local anaesthetic.
Diagnosis
There is no gold standard diagnostic method. The diagnosis can be considered by tenderness over the iliac crest or LPSL causing provocation of symptoms. Pain relief following local anaesthetic injection can give further weight to the diagnosis.
The SCN tender point is typically on the posterior iliac crest, approximately 70mm from the midline and 45mm from the PSIS. The MCN tender point is typically on the LPSL within 40mm caudal to the PSIS.
Treatment
Injections
Trigger point injections have been described.
Surgery
Reports have been published on SCN release and MCN release. Most reports are on SCN release.
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


