Superior Cluneal Nerve Entrapment: Difference between revisions
No edit summary |
No edit summary |
||
| Line 7: | Line 7: | ||
[[File:Superior and middle cluneal nerves.jpg|thumb|right|Superior and middle cluneal nerves with typical entrapment sites. Multiple branches of the superior cluneal nerves can be entrapped where they pierce the thoracolumbar fascia over the iliac crest. Middle cluneal nerve entrapment can occur where it passes under or through the long posterior sacroiliac ligament.{{#pmid:27004164|Aota}}]] | [[File:Superior and middle cluneal nerves.jpg|thumb|right|Superior and middle cluneal nerves with typical entrapment sites. Multiple branches of the superior cluneal nerves can be entrapped where they pierce the thoracolumbar fascia over the iliac crest. Middle cluneal nerve entrapment can occur where it passes under or through the long posterior sacroiliac ligament.{{#pmid:27004164|Aota}}]] | ||
Superior cluneal nerve (SCN) entrapment occurs where the nerve pierces the thoracolumbar attachment at the posterior iliac crest. Typically it has been described based on cadaver studies that the medial branch of the SCN consistently passes through an osteofibrous tunnel and can be spontaneously entrapped. Kuniya et al found that in their 19 subjects requiring SCN release, they did not find severe constriction within a bony groove on the iliac crest, but they found at least two SCN branches passing underneath a mixture of superficial thoracolumbar and gluteal fascia at the point of attachment to the iliac crest. <ref name="kuniya"/> | Superior cluneal nerve (SCN) entrapment occurs where the nerve pierces the thoracolumbar attachment at the posterior iliac crest. Typically it has been described based on cadaver studies that the medial branch of the SCN consistently passes through an osteofibrous tunnel and can be spontaneously entrapped. Kuniya et al found that in their 19 subjects requiring SCN release, they did not find severe constriction within a bony groove on the iliac crest, but they found at least two SCN branches passing underneath a mixture of superficial thoracolumbar and gluteal fascia at the point of attachment to the iliac crest. <ref name="kuniya"/> | ||
The prevalence of vertebral compression fractures is higher in those with SCN than in those without SCN disorder (26% vs 12%), most commonly at T12-L3. It is theorised that this causes a sagittal imbalance with increased kyphosis of the spine, thereby irritating the SCN at its origin from unstable facet joints or by stretching the SCN itself.<ref name="kuniya"/> | |||
The middle cluneal nerve (MCN) is comprised of the sensory branches of the S1 to S3 dorsal rami. It travels below the PSIS in an approximately horizontal route and supplies the skin overlying the posteromedial buttock. The S1 to S2 composition could explain why some patients may get leg symptoms. It can become trapped with passing underneith or through the long posterior sacroiliac ligament. MCN entrapment can be confused with sacroiliac joint pain. Even a positive sacroiliac joint block could still indicate LPSL pain or MCN entrapment if there is dorsal extravasation of the local anaesthetic. | The middle cluneal nerve (MCN) is comprised of the sensory branches of the S1 to S3 dorsal rami. It travels below the PSIS in an approximately horizontal route and supplies the skin overlying the posteromedial buttock. The S1 to S2 composition could explain why some patients may get leg symptoms. It can become trapped with passing underneith or through the long posterior sacroiliac ligament. MCN entrapment can be confused with sacroiliac joint pain. Even a positive sacroiliac joint block could still indicate LPSL pain or MCN entrapment if there is dorsal extravasation of the local anaesthetic. | ||
| Line 14: | Line 16: | ||
==Clinical Features== | ==Clinical Features== | ||
In those with SCN disorder, around 50% have leg symptoms, but only 1% have leg symptoms only. The most commonly aggravating features are walking, rising from sitting, and standing. | In those with SCN disorder, around 50% have leg symptoms, but only 1% have leg symptoms only. The most commonly aggravating features are walking, rising from sitting, and standing. | ||
==Diagnosis== | ==Diagnosis== | ||
| Line 39: | Line 41: | ||
===Surgery=== | ===Surgery=== | ||
Reports have been published on SCN release and MCN release. Most reports are on SCN release. In Kuniya's study, approximately 20% of patients proceeded to SCN decompression due to failure of having long term relief from repeated SCN nerve blocks. | Reports have been published on SCN release and MCN release. Most reports are on SCN release. In Kuniya's study, approximately 20% of patients proceeded to SCN decompression due to failure of having long term relief from repeated SCN nerve blocks. Predictors of success were pain duration less than 3 years, and consistently having relief for three days or more from SCN blocks. | ||
==References== | ==References== | ||
Revision as of 14:15, 7 September 2020
Some authors posit that cluneal nerve entrapment is an under-diagnosed cause of chronic low back and leg pain, and it can cause neuropathic type symptoms. Superior cluneal nerve entrapment is thought to be more common than middle cluneal nerve entrapment. The best research paper on SCN entrapment that I have come across is by Kuniya et al, which is open access and a highly recommended read. [1]
Anatomy and Pathophysiology
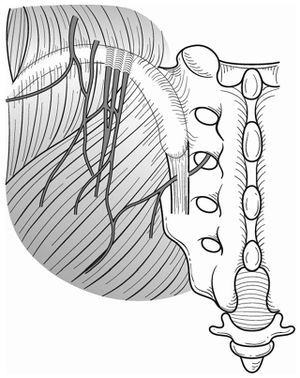
Superior cluneal nerve (SCN) entrapment occurs where the nerve pierces the thoracolumbar attachment at the posterior iliac crest. Typically it has been described based on cadaver studies that the medial branch of the SCN consistently passes through an osteofibrous tunnel and can be spontaneously entrapped. Kuniya et al found that in their 19 subjects requiring SCN release, they did not find severe constriction within a bony groove on the iliac crest, but they found at least two SCN branches passing underneath a mixture of superficial thoracolumbar and gluteal fascia at the point of attachment to the iliac crest. [1]
The prevalence of vertebral compression fractures is higher in those with SCN than in those without SCN disorder (26% vs 12%), most commonly at T12-L3. It is theorised that this causes a sagittal imbalance with increased kyphosis of the spine, thereby irritating the SCN at its origin from unstable facet joints or by stretching the SCN itself.[1]
The middle cluneal nerve (MCN) is comprised of the sensory branches of the S1 to S3 dorsal rami. It travels below the PSIS in an approximately horizontal route and supplies the skin overlying the posteromedial buttock. The S1 to S2 composition could explain why some patients may get leg symptoms. It can become trapped with passing underneith or through the long posterior sacroiliac ligament. MCN entrapment can be confused with sacroiliac joint pain. Even a positive sacroiliac joint block could still indicate LPSL pain or MCN entrapment if there is dorsal extravasation of the local anaesthetic.
Epidemiology
In one retrospective review of 834 patient with LBP, 14% were thought to be due to superior cluneal nerve entrapment. See the diagnosis section below for their diagnostic method.[1]
Clinical Features
In those with SCN disorder, around 50% have leg symptoms, but only 1% have leg symptoms only. The most commonly aggravating features are walking, rising from sitting, and standing.
Diagnosis
- Superior cluneal nerve entrapment
There is no agreed diagnostic method. The diagnosis can be considered by tenderness over the iliac crest or LPSL causing provocation of symptoms. Pain relief following local anaesthetic injection can give further weight to the diagnosis.
Kuniya et al used the following diagnostic criteria. [1]
- Maximal tender point on posterior iliac crest approximately 70 mm from the midline and 45 mm from the PSIS where the medial branch of the SCN runs through an osteofibrous tunnel consisting of the thoraco-lumbar fascia and the iliac crest and
- Palpation of the maximally tender point reproduced the chief complaint of LBP and/or leg symptoms
In their study, when patients met both criteria, a nerve block injection was performed. 62% of patients had a 50% decrease of VAS after the first injection, 67% after the second injection, and 68% after the third injection.
If relief of symptoms is obtained following injection that can give further weight to the diagnosis. In their study, if repeated injections failed to relieve symptoms then they had SCN decompression.
- Middle cluneal nerve entrapment
Again there is no agreed diagnostic method. The MCN tender point is typically on the LPSL within 40mm caudal to the PSIS.
Treatment
Injections
Trigger point injections have been described. Kuniya et al reported a very rare risk of erectile dysfunction following injections to the SCN.
Surgery
Reports have been published on SCN release and MCN release. Most reports are on SCN release. In Kuniya's study, approximately 20% of patients proceeded to SCN decompression due to failure of having long term relief from repeated SCN nerve blocks. Predictors of success were pain duration less than 3 years, and consistently having relief for three days or more from SCN blocks.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Kuniya et al.. Prospective study of superior cluneal nerve disorder as a potential cause of low back pain and leg symptoms. Journal of orthopaedic surgery and research 2014. 9:139. PMID: 25551470. DOI. Full Text.
- ↑ Aota. Entrapment of middle cluneal nerves as an unknown cause of low back pain. World journal of orthopedics 2016. 7:167-70. PMID: 27004164. DOI. Full Text.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


