Talocalcaneal Joint (Subtalar Joint)
{{{{{quality}}}}}
| |
| Talocalcaneal Joint (Subtalar Joint) | |
|---|---|
| Primary Type | Triplanar"Triplanar" is not in the list (Synovial Joint, Cartilaginous Joint, Fibrous Joint, Compound Joint) of allowed values for the "Has joint type" property., uniaxial joint"Uniaxial joint" is not in the list (Synovial Joint, Cartilaginous Joint, Fibrous Joint, Compound Joint) of allowed values for the "Has joint type" property. |
| Secondary Type | |
| Bones | Talus and Calcaneus"Talus and Calcaneus" is not in the list (Vertebra, Sacrum, Coccyx, Scapula, Clavicle, Humerus, Radius, Ulna, Scaphoid, Lunate, ...) of allowed values for the "Has joint bones" property. |
| Ligaments | Multiple, interosseous talocalcaneal ligament is most important |
| Muscles | |
| Innervation | Medial plantar, lateral plantar, and deep fibular nerves |
| Vasculature | Posterior tibial and fibular arteries |
| ROM | Inversion (25° to 30°), eversion (5° to 10°) |
| Volume | |
| Conditions | |
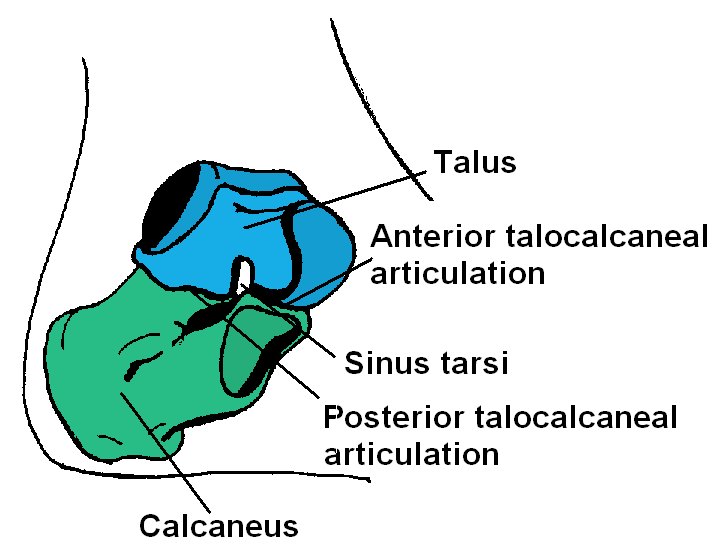
The talocalcaneal joint, also called the clinical subtalar joint, is an important and complex joint in the hindfoot that allows articulation of the talus and calcaneus.
Articulations
The calcaneus forms a triplanar, uniaxial joint with the talus.
- Anteriorly, the talus sits on the anterior and middle facets of the calcaneus, forming the acetabulum pedis with the posterior surface of the navicular bone.
- Posteriorly the concave facet of the talus sits on the convex posterior facet of the calcaneus
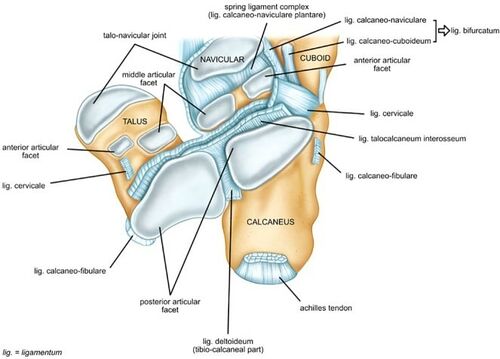
The anterior and middle facets are concave; while the posterior facet is convex. The anterior facet sits just lateral to the medial facet. The posterior facet is the largest of the three. It is separated from the other two facets by the interosseous calcaneal ligament.
The anterior talo-calcaneal articulation (anterior and middle facets) are often congruent and are part of a separate synovial cavity (talocalcaneonavicular joint) to the posterior talocalcaneal articulation. The posterior talocalcaneal articulation (posterior facet) only, comprises the anatomical subtalar joint.
The three calcaneal facets vary in their shape between individuals. Variations are common and include combined anterior and middle facets in ovoid form in 42%, bean form in 22%, and complete separation in 36%.
The sustenataculum tali is comprised of the dorsal surface of the middle calcaneal facet. It allows slides of the tibialis posterior, flexor hallucis longus, and flexor digitorum longus tendons.[1]
Ligaments
There are a number of ligaments.
- Intrinsic
- Cervical ligament
- Interosseous talocalcaneal ligament: This is the key ligament. It is strong, thick ligaments that extends from the articular facets of the inferior talus to the superior surface of the calcaneus.
- Extrinsic
- Calcaneofibular part of the lateral collateral ligament
- Tibiocalcaneal ligament of the deltoid
- Lateral talocalcaneal ligament: relatively weak
- Anterior talocalcaneal ligament: relatively weak
The interosseous ligament if dysfunctional, especially in combination with anterior talo-fibular ligament failure, results in abnormal anterolateral rotation of the talus during walking. This leads to subtalar joint and secondary ankle joint instability.
The extensor tendons influence subtalar joint stability and movement. The inferior extensor retinaculum is important here for tendon function as it acts like a pulley. There is also support from the tendons of peroneus longus, peroneus brevis, flexor hallucis longus, tibialis posterior, and flexor digitorum longus.
The calcaneus receives additional support through articulation with the navicular bone and by the spring ligament. The spring ligament is important in stabilising the head of the talus. Spring ligament insufficiency can lead to acquired flat foot deformity.
Movement
Subtalar joint movement is very complex. The geometry of the joint allows inversion (25° to 30°) and eversion (5° to 10°) of the ankle, and most of eversion and inversion of the foot occurs here. Anteroposterior and mediolateral translation also occur but aren't able to be assessed clinically. The position of the ankle affects subtalar joint movement, e.g. dorsal extension of the ankle joint reduces subtalar movement.
Evertors: extensor hallucis longus, extensor digitorum longus, peroneus longus (strongest evertor), and peroneus brevis
Invertors: tibialis posterior (strongest invertor), flexor digitorum longus, flexor hallucis longus and tibialis anterior.
Triceps surae has a slight inversion function while the ankle joint is in flexion/inversion and may change to an evertor when the subtalar joint is in eversion.
Neurovascular Supply
The joint is supplied by two arteries and two nerves.
Arteries: Posterior tibial and fibular arteries
Nerves: The plantar aspect of the joint is innervated by the medial or lateral plantar nerve. The dorsal aspect of the joint is supplied by the deep fibular nerve.
References
- https://radiopaedia.org/articles/talocalcaneal-joint
- Brockett, Claire L, and Graham J Chapman. “Biomechanics of the ankle.” Orthopaedics and trauma vol. 30,3 (2016): 232-238. doi:10.1016/j.mporth.2016.04.015

