Femoroacetabular Impingement: Difference between revisions
Tag: Undo |
No edit summary |
||
| (8 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{Authors}} | {{Authors|Authors=Jeremy}} | ||
{{Condition | {{Condition | ||
|quality= | |quality=Partial | ||
|image=Femoral acetabular impingement FAI.svg | |image=Femoral acetabular impingement FAI.svg | ||
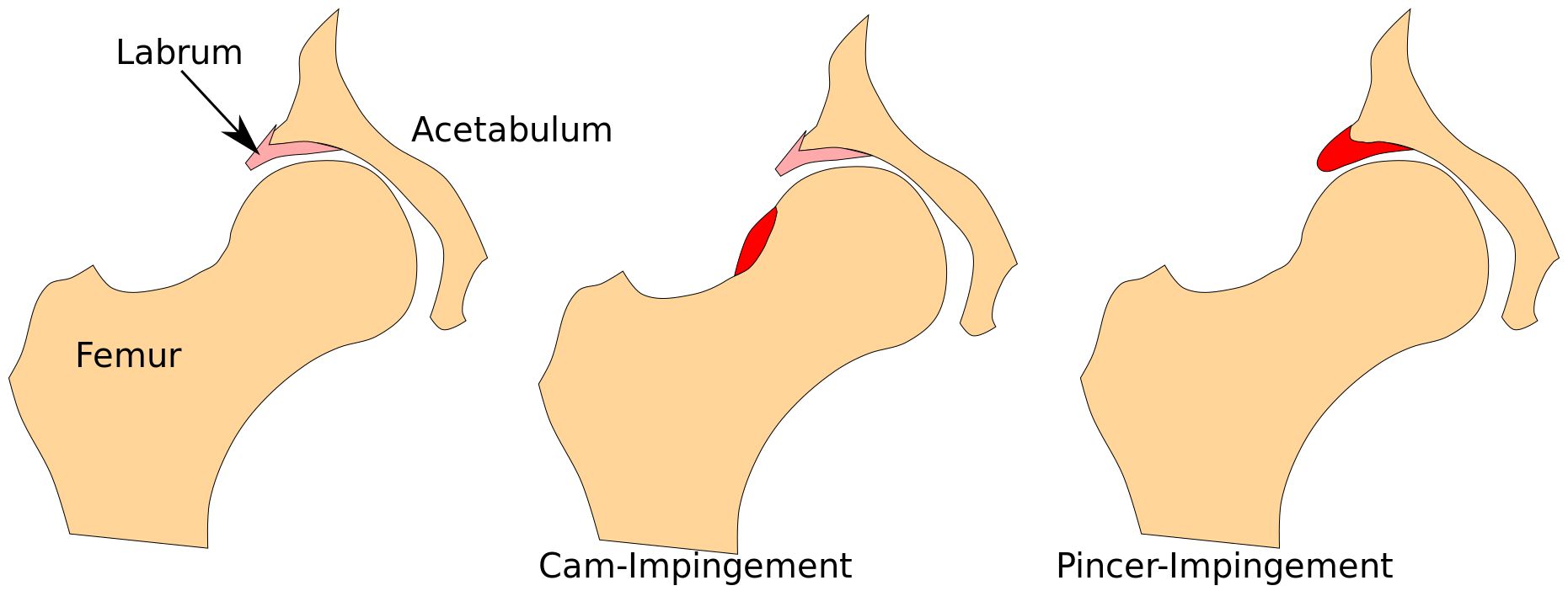
|caption=Normal, CAM, and pincer morphologies. | |caption=Normal, CAM, and pincer morphologies. | ||
|definition=Pathological contact between the femoral head-neck junction and the acetabular rim during functional hip movement | |||
|classification=CAM, Pincer, or mixed | |||
|riskfactors=Dose-response relationship between intense sporting activity during adolescence and CAM morphology. | |||
|clinicalfeatures=Insidious mild positional or movement related groin pain. | |||
|diagnosis=Presence of cam and/or pincer morphology on imaging in the appropriate clinical picture. | |||
|tests=Plain films and MRI | |||
|taxonomy=Called femoroacetabular impingement syndrome in the presence of symptoms. | |||
|treatment=Exercise, physiotherapy, surgery. | |||
|prognosis=Risk factor for [[Hip Osteoarthritis|hip osteoarthritis]] | |||
}} | }} | ||
'''Femoroacetabular impingement''' (FAI) refers to abnormally shaped femoral head and neck junction and/or acetabulum. This creates a space conflict with hip flexion. It is a risk factor for early onset [[Hip Osteoarthritis|hip osteoarthritis]], but is not a sufficient cause. | '''Femoroacetabular impingement''' (FAI) refers to abnormally shaped femoral head and neck junction and/or acetabulum. This creates a space conflict with hip flexion. It is a risk factor for early onset [[Hip Osteoarthritis|hip osteoarthritis]], but is not a sufficient cause. | ||
==Classification== | ==Classification== | ||
There are two patterns, cam and pincer, as well as a combination of both types. In cam FAI there is a thickened, aspherical femoral head-neck junction, which abuts against the anterosuperior labrum with hip flexion, and results in compression of the labrum and acetabular cartilage. This leads to separation of the labrum from the acetabular cartilage and delamination of the acetabular cartilage from the subchondral bone.<ref name=":0">{{Cite journal|last=Murphy|first=Nicholas J.|last2=Eyles|first2=Jillian P.|last3=Hunter|first3=David J.|date=2016-11|title=Hip Osteoarthritis: Etiopathogenesis and Implications for Management|url=https://pubmed.ncbi.nlm.nih.gov/27671326|journal=Advances in Therapy|volume=33|issue=11|pages=1921–1946|doi=10.1007/s12325-016-0409-3|issn=1865-8652|pmc=5083776|pmid=27671326}}</ref> | |||
In pincer FAI, there is an overcoverage of the acetabulum with a deepened acetabular on the femoral head. The femoral neck abuts against the acetabular labrum and compresses it, damaging both the labrum and underlying cartilage. Lesions usually occur anterosuperiorly from hip flexion like with cam lesions, but also posteroinferiorly from posterior subluxation due to continued flexion causing a contre-coup lesion. | In pincer FAI, there is an overcoverage of the acetabulum with a deepened acetabular on the femoral head. The femoral neck abuts against the acetabular labrum and compresses it, damaging both the labrum and underlying cartilage. Lesions usually occur anterosuperiorly from hip flexion like with cam lesions, but also posteroinferiorly from posterior subluxation due to continued flexion causing a contre-coup lesion. | ||
<gallery widths=300 heights=200> | |||
Pincer impingement.jpg|Pincer impingement. There is acetabular over-coverage, and the femoral neck abuts against the labrum, damaging it as well as the underlying cartilage. With continued hip flexion there is subtle joint subluxation and a contre-coup lesion forms. There is delamination of the labrum from the acetabular cartilage.<ref name=":0" /> | |||
Cam impingement.jpg|Cam impingement. The cam lesion abuts against the labrum, pushing it outwards and compressing the acetabular cartilage inwards. The labrum separates from the cartilage and the acetabular cartilage delaminates from the bone.<ref name=":0" /> | |||
</gallery> | |||
==Clinical Features== | ==Clinical Features== | ||
The pain is often insidious with mild groin pain that occurs over many years and then suddenly worsens. The patient often uses a C grip with their index finger and thumb proximal to the greater trochanter to indicate the painful region. The pain is most noticeable when sitting with the hips flexed to 90 degrees for long periods and reduces with standing. There may be additional pain in the back or thigh. The patient may describe mechanical symptoms such as catching, stiffness, or restricted motion. In the presence of an associated [[Hip Labral Tear|labral tear]] there may be sharp pain with catching sensations. | |||
There may be limited flexion or internal rotation of the hip and provocation of groin pain with FADDIR test. The flexion internal rotation test may also be positive. However both of these tests are sensitive but not specific. | |||
== Differential Diagnosis == | |||
{{DDX Box|ddx-text={{Hip Pain DDX}}}} | |||
== Imaging == | |||
Obtain AP and lateral plain films. See [[Hip Radiograph]] for measurements. MRI is the definitive scan. | |||
==Prognosis== | ==Prognosis== | ||
The CHECK study assessed 1002 patients aged 45–65 years with early symptoms of hip OA but without definite radiographic evidence of the same over 5 years. At baseline, 76% of the included hips had no radiographic signs of osteoarthritis and 24% doubtful osteoarthritis. Cam deformities and acetabular dysplasia were shown to be associated with an increased [[Odds Ratio|odds ratio]] for progression to early onset osteoarthritis.<ref>{{Cite journal|last=Agricola|first=Rintje|last2=Heijboer|first2=Marinus P.|last3=Bierma-Zeinstra|first3=Sita M. A.|last4=Verhaar|first4=Jan A. N.|last5=Weinans|first5=Harrie|last6=Waarsing|first6=Jan H.|date=2013-06|title=Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK)|url=https://pubmed.ncbi.nlm.nih.gov/22730371|journal=Annals of the Rheumatic Diseases|volume=72|issue=6|pages=918–923|doi=10.1136/annrheumdis-2012-201643|issn=1468-2060|pmid=22730371}}</ref> While pincer changes were actually associated with a ''reduced'' risk.<ref>{{Cite journal|last=Agricola|first=R.|last2=Heijboer|first2=M. P.|last3=Roze|first3=R. H.|last4=Reijman|first4=M.|last5=Bierma-Zeinstra|first5=S. M. A.|last6=Verhaar|first6=J. a. N.|last7=Weinans|first7=H.|last8=Waarsing|first8=J. H.|date=2013-10|title=Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK)|url=https://pubmed.ncbi.nlm.nih.gov/23850552|journal=Osteoarthritis and Cartilage|volume=21|issue=10|pages=1514–1521|doi=10.1016/j.joca.2013.07.004|issn=1522-9653|pmid=23850552}}</ref> | The CHECK study assessed 1002 patients aged 45–65 years with early symptoms of hip OA but without definite radiographic evidence of the same over 5 years. At baseline, 76% of the included hips had no radiographic signs of osteoarthritis and 24% doubtful osteoarthritis. Cam deformities and acetabular dysplasia were shown to be associated with an increased [[Odds Ratio|odds ratio]] for progression to early onset osteoarthritis.<ref>{{Cite journal|last=Agricola|first=Rintje|last2=Heijboer|first2=Marinus P.|last3=Bierma-Zeinstra|first3=Sita M. A.|last4=Verhaar|first4=Jan A. N.|last5=Weinans|first5=Harrie|last6=Waarsing|first6=Jan H.|date=2013-06|title=Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK)|url=https://pubmed.ncbi.nlm.nih.gov/22730371|journal=Annals of the Rheumatic Diseases|volume=72|issue=6|pages=918–923|doi=10.1136/annrheumdis-2012-201643|issn=1468-2060|pmid=22730371}}</ref> While pincer changes were actually associated with a ''reduced'' risk.<ref>{{Cite journal|last=Agricola|first=R.|last2=Heijboer|first2=M. P.|last3=Roze|first3=R. H.|last4=Reijman|first4=M.|last5=Bierma-Zeinstra|first5=S. M. A.|last6=Verhaar|first6=J. a. N.|last7=Weinans|first7=H.|last8=Waarsing|first8=J. H.|date=2013-10|title=Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK)|url=https://pubmed.ncbi.nlm.nih.gov/23850552|journal=Osteoarthritis and Cartilage|volume=21|issue=10|pages=1514–1521|doi=10.1016/j.joca.2013.07.004|issn=1522-9653|pmid=23850552}}</ref> | ||
There is also risk for development of [[Hip Labral Tear|labral tears]]. | |||
==Resources== | |||
{{Members link}} | |||
==References== | |||
[[Category:Pelvis, Hip and Thigh Conditions]] | [[Category:Pelvis, Hip and Thigh Conditions]] | ||
<references /> | <references /> | ||
{{References}} | {{References}} | ||
{{Reliable sources}} | {{Reliable sources}} | ||
[[Category:Developmental Disorders]] | |||
Latest revision as of 21:59, 17 April 2022
| |
| Femoroacetabular Impingement | |
|---|---|
| Definition | Pathological contact between the femoral head-neck junction and the acetabular rim during functional hip movement |
| Classification | CAM, Pincer, or mixed |
| Risk Factors | Dose-response relationship between intense sporting activity during adolescence and CAM morphology. |
| Clinical Features | Insidious mild positional or movement related groin pain. |
| Diagnosis | Presence of cam and/or pincer morphology on imaging in the appropriate clinical picture. |
| Tests | Plain films and MRI |
| Taxonomy | Called femoroacetabular impingement syndrome in the presence of symptoms. |
| Treatment | Exercise, physiotherapy, surgery. |
| Prognosis | Risk factor for hip osteoarthritis |
Femoroacetabular impingement (FAI) refers to abnormally shaped femoral head and neck junction and/or acetabulum. This creates a space conflict with hip flexion. It is a risk factor for early onset hip osteoarthritis, but is not a sufficient cause.
Classification
There are two patterns, cam and pincer, as well as a combination of both types. In cam FAI there is a thickened, aspherical femoral head-neck junction, which abuts against the anterosuperior labrum with hip flexion, and results in compression of the labrum and acetabular cartilage. This leads to separation of the labrum from the acetabular cartilage and delamination of the acetabular cartilage from the subchondral bone.[1]
In pincer FAI, there is an overcoverage of the acetabulum with a deepened acetabular on the femoral head. The femoral neck abuts against the acetabular labrum and compresses it, damaging both the labrum and underlying cartilage. Lesions usually occur anterosuperiorly from hip flexion like with cam lesions, but also posteroinferiorly from posterior subluxation due to continued flexion causing a contre-coup lesion.
Pincer impingement. There is acetabular over-coverage, and the femoral neck abuts against the labrum, damaging it as well as the underlying cartilage. With continued hip flexion there is subtle joint subluxation and a contre-coup lesion forms. There is delamination of the labrum from the acetabular cartilage.[1]
Cam impingement. The cam lesion abuts against the labrum, pushing it outwards and compressing the acetabular cartilage inwards. The labrum separates from the cartilage and the acetabular cartilage delaminates from the bone.[1]
Clinical Features
The pain is often insidious with mild groin pain that occurs over many years and then suddenly worsens. The patient often uses a C grip with their index finger and thumb proximal to the greater trochanter to indicate the painful region. The pain is most noticeable when sitting with the hips flexed to 90 degrees for long periods and reduces with standing. There may be additional pain in the back or thigh. The patient may describe mechanical symptoms such as catching, stiffness, or restricted motion. In the presence of an associated labral tear there may be sharp pain with catching sensations.
There may be limited flexion or internal rotation of the hip and provocation of groin pain with FADDIR test. The flexion internal rotation test may also be positive. However both of these tests are sensitive but not specific.
Differential Diagnosis
- Anterior pain
- Hip Osteoarthritis
- Femoroacetabular Impingement
- Iliopsoas Tendionopathy
- Inflammatory arthritis
- Avascular necrosis/osteonecrosis of the femoral head
- Hip Labral Tear
- Nerve Entrapments: Genitofemoral Nerve Entrapment, Ilioinguinal Nerve Entrapment
- Developmental Dysplasia of the Hip
- Transient Osteoporosis of the Hip
- Inguinal or femoral hernia
- Gynaecological causes
- Gonadal tumours
- Inguinal lymphadenopathy
- Posterior pain
- Lateral pain
- Medial pain
- Other
- Septic Arthritis
- Hip Fracture
- Hip chondral defects
- Ligamentum teres injury
- Pelvic bone tumours
- Pelvic insufficiency fractures
- Stress fracture
- Peripheral Vascular Disease
- Fibromyalgia
- Leaking abdominal aortic aneurysm
Imaging
Obtain AP and lateral plain films. See Hip Radiograph for measurements. MRI is the definitive scan.
Prognosis
The CHECK study assessed 1002 patients aged 45–65 years with early symptoms of hip OA but without definite radiographic evidence of the same over 5 years. At baseline, 76% of the included hips had no radiographic signs of osteoarthritis and 24% doubtful osteoarthritis. Cam deformities and acetabular dysplasia were shown to be associated with an increased odds ratio for progression to early onset osteoarthritis.[2] While pincer changes were actually associated with a reduced risk.[3]
There is also risk for development of labral tears.
Resources
References
- ↑ 1.0 1.1 1.2 Murphy, Nicholas J.; Eyles, Jillian P.; Hunter, David J. (2016-11). "Hip Osteoarthritis: Etiopathogenesis and Implications for Management". Advances in Therapy. 33 (11): 1921–1946. doi:10.1007/s12325-016-0409-3. ISSN 1865-8652. PMC 5083776. PMID 27671326. Check date values in:
|date=(help) - ↑ Agricola, Rintje; Heijboer, Marinus P.; Bierma-Zeinstra, Sita M. A.; Verhaar, Jan A. N.; Weinans, Harrie; Waarsing, Jan H. (2013-06). "Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK)". Annals of the Rheumatic Diseases. 72 (6): 918–923. doi:10.1136/annrheumdis-2012-201643. ISSN 1468-2060. PMID 22730371. Check date values in:
|date=(help) - ↑ Agricola, R.; Heijboer, M. P.; Roze, R. H.; Reijman, M.; Bierma-Zeinstra, S. M. A.; Verhaar, J. a. N.; Weinans, H.; Waarsing, J. H. (2013-10). "Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK)". Osteoarthritis and Cartilage. 21 (10): 1514–1521. doi:10.1016/j.joca.2013.07.004. ISSN 1522-9653. PMID 23850552. Check date values in:
|date=(help)
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,
![Pincer impingement. There is acetabular over-coverage, and the femoral neck abuts against the labrum, damaging it as well as the underlying cartilage. With continued hip flexion there is subtle joint subluxation and a contre-coup lesion forms. There is delamination of the labrum from the acetabular cartilage.[1]](/w/img_auth.php/thumb/1/1b/Pincer_impingement.jpg/300px-Pincer_impingement.jpg)
![Cam impingement. The cam lesion abuts against the labrum, pushing it outwards and compressing the acetabular cartilage inwards. The labrum separates from the cartilage and the acetabular cartilage delaminates from the bone.[1]](/w/img_auth.php/thumb/7/7f/Cam_impingement.jpg/300px-Cam_impingement.jpg)


