◒
Greater Occipital Nerve Injection
From WikiMSK
This article is still missing information.
| Greater Occipital Nerve Injection | |
|---|---|
| Indication | Occipital Neuralgia |
| Syringe | 3mL |
| Needle | 27-30G |
| Steroid | optional 4mg dexamethasone'"`UNIQ--ref-00000001-QINU`"' |
| Local | 1-3mL of anaesthetic |
| Volume | 1-3mL |
Anatomy
The greater occipital nerve (GON) arises from the medial branches of the posterior ramus of the second cervical spinal nerve. The nerve arises between the axis and atlas, and emerges from the suboccipital triangle. It innervates the occipital area from the superior nuchal line to the vertex. It then proceeds superolaterally in multiple branches.
Background
- Therapeutic and diagnostic for occipital neuralgia
- Usually performed by targeting the tender points that approximate the affected branches of the C2 nerve, either the greater or lesser occipital nerve.
- The greater occipital nerve is 2cm inferior and lateral to the external occipital protuberance, and is between ~8-18 mm deep[2]. It can also be identified at one third of the distance from the external occipital protuberance to the mastoid process.
- The lesser occipital nerve is 5cm lateral to the external occipital protuberance.
Indications
- Suspected or confirmed occipital neuralgia
- Migraine refractory to conservative treatment
- Post-lumbar puncture headache refractory to conservative treatment
- Cluster headache, occipital neuralgia, cervicogenic headache, or migraine with occipital nerve irritation or tenderness [3]
Contraindications
- Infection overlying injection site
Procedure
Ultrasound Guided
- In-plane technique
- Prone, side-lying, or seated position with the head slightly flexed.
- Stand contralateral to the injection site, in line with the transducer and with the ultrasound screen on the opposite side
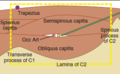
- Using a high-frequency linear array transducer, localize the C2 spinous process which is bifid. The C1 spinous process is not bifid.
- Slide the probe laterally (away from yourself) towards the ipsilateral lamina of C2.
- Rotate the lateral part of the transducer cephalad until the transverse process of C1 is visualized (around 20–30 degrees).
- Identify the muscular tissue planes and the greater occipital nerve
- Colour doppler can be used to identify the occipital artery which lies just medial to the greater occipital nerve
- Insert the needle in-plane from medial to lateral and advance until the needle tip is close to the nerve.
See Palamar et al for a review on technique[4].
Non-ultrasound Guided
- Patient in position of comfort allowing access to posterior head and neck. (laying prone or sitting with head down in arms)
- Identify Greater Occipital Nerve (GON), which may be palpated 1.5-2.5 cm inferior to occipital protuberance and ~1.5-2 cm lateral to midline[5]
- Cleanse skin with betadine or chlorhexidine and allow to dry
- Insert needle over nerve at 90 degrees to skin until hit bone, then withdraw slightly[6]
- Aspirate to ensure not in vessel.
- Inject ~1-3 mL of local anesthetic. (may inject small amount medial and lateral to nerve to ensure adequate block)[1]
- Repeat on contralateral side, if indicated.
Maximum Doses of Anesthetic Agents
| Agent | Without Adrenaline | With Adrenaline | Duration | Notes |
| Lidocaine | 5 mg/kg (max 300mg) | 7 mg/kg (max 500mg) | 30-90 min |
|
| Mepivicaine | 7 mg/kg | 8 mg/kg | ||
| Bupivicaine | 2.5 mg/kg (max 175mg) | 3 mg/kg (max 225mg) | 6-8 hr |
|
| Ropivacaine | 3 mg/kg | |||
| Prilocaine | 6 mg/kg | |||
| Tetracaine | 1 mg/kg | 1.5 mg/kg | 3hrs (10hrs with epi) | |
| Procaine | 7 mg/kg | 10 mg/kg | 30min (90min with epi) |
Complications
Complications are rare due to superficial location and lack of major surrounding structures.[1]
- Damage to surrounding structures
- Bleeding
- Infection
- Repeated blocks with steroid may result in transient dizziness or elevated blood pressure, and the patient may rarely become cushingoid.
Aftercare
- The procedure may be repeated if pain recurs
See Also
References
- ↑ 1.0 1.1 1.2 Brock G. The occasional greater occipital nerve block. Can J Rural Med. 2014 Fall;19(4):152-5.
- ↑ M. Greher, B. Moriggl, M. Curatolo, L. Kirchmair and U. Eichenberger. Sonographic visualization and ultrasound-guided blockade of the greater occipital nerve: a comparison of two selective techniques confirmed by anatomical dissection. Br. J. Anaesth. (2010) 104 (5): 637-642.
- ↑ https://www.nuemblog.com/blog/occipital-nerve-block
- ↑ Palamar D, Uluduz D, Saip S, et al. Ultrasound-guided greater occipital nerve block: an efficient technique in chronic refractory migraine without aura? Pain Physician. 2015 Mar-Apr;18(2):153-62.
- ↑ Dach F, Éckeli ÁL, Ferreira Kdos S, Speciali JG. Nerve block for the treatment of headaches and cranial neuralgias - a practical approach. Headache. 2015 Feb;55 Suppl 1:59-71.
- ↑ Inan LE, Inan N, Karadaş Ö, et al. Greater occipital nerve blockade for the treatment of chronic migraine: a randomized, multicenter, double-blind, and placebo-controlled study. Acta Neurol Scand. 2015 Mar 13. doi: 10.1111/ane.12393
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,