Hip Osteoarthritis: Difference between revisions
No edit summary |
|||
| Line 121: | Line 121: | ||
!Sensitivity | !Sensitivity | ||
!Specificity | !Specificity | ||
!LR+ | !LR+ (95% CI) | ||
!LR- | !LR-(95% CI) | ||
|- | |- | ||
|Abductor weakness | |Abductor weakness | ||
| Line 273: | Line 273: | ||
!Findings | !Findings | ||
!Number of findings | !Number of findings | ||
!+ | !LR+ (95% CI) | ||
|- | |- | ||
| rowspan="3" | | | rowspan="3" | | ||
Revision as of 19:11, 20 June 2021
Epidemiology
A US study of mostly Caucasian people aged over 50, the prevalence of radiographic hip OA was 19.6%, and the prevalence of symptomatic disease was 4.2%, with the prevalence increasing with higher age. The authors found a male predominance of symptomatic OA, especially in older individuals, unlike other studies which have tended to find a female predominance. There is generally a male predominance of radiographic OA.[1] A Japanese study found the prevalence of radiographic hip osteoarthritis to be 18.2% in men and 14.3% in women[2]
The prevalence of hip OA in patients with hip and/or groin pain presenting to primary care is 35%.[3]
| Radiographic Hip OA (95% Cl) | Symptomatic Hip OA (95% Cl) | |
|---|---|---|
| Men (n=434) | 24.7% (20.6%-28.7%) | 5.2% (3.3%-7.8%) |
| Women (n=544) | 13.6% (10.7%-16.5%) | 3.0% (1.7%-4.8%) |
| Age 50-59 (n=390) | 14.6% (11.1%-18.1%) | 3.4% (1.8%-5.8%) |
| Age 60-69 (n=337) | 16.6% (12.6%-20.6%) | 2.7% (1.3%-5.1%) |
| Age 70-79 (n=197) | 25.9% (19.8%-32.0%) | 6.3% (3.3%-10.7%) |
| Age ≥ 80 (n=54) | 31.5% (19.1%-43.9%) | 7.4% (0.2%-17.9%) |
| Crude Prevalence | 18.5% (16.1%-20.9%) | 4.0% (2.8%-5.4%) |
| Age-standardized Prevalence | 19.6% (16.7%-23.0%) | 4.2% (2.9%-6.1%) |
Aetiology
Femoroacetabular impingement (FAI) and the less common developmental dysplasia of the hip (DDH) are hip joint morphology abnormalities that are associated with early onset hip OA. However, FAI is also common in asymptomatic individuals.
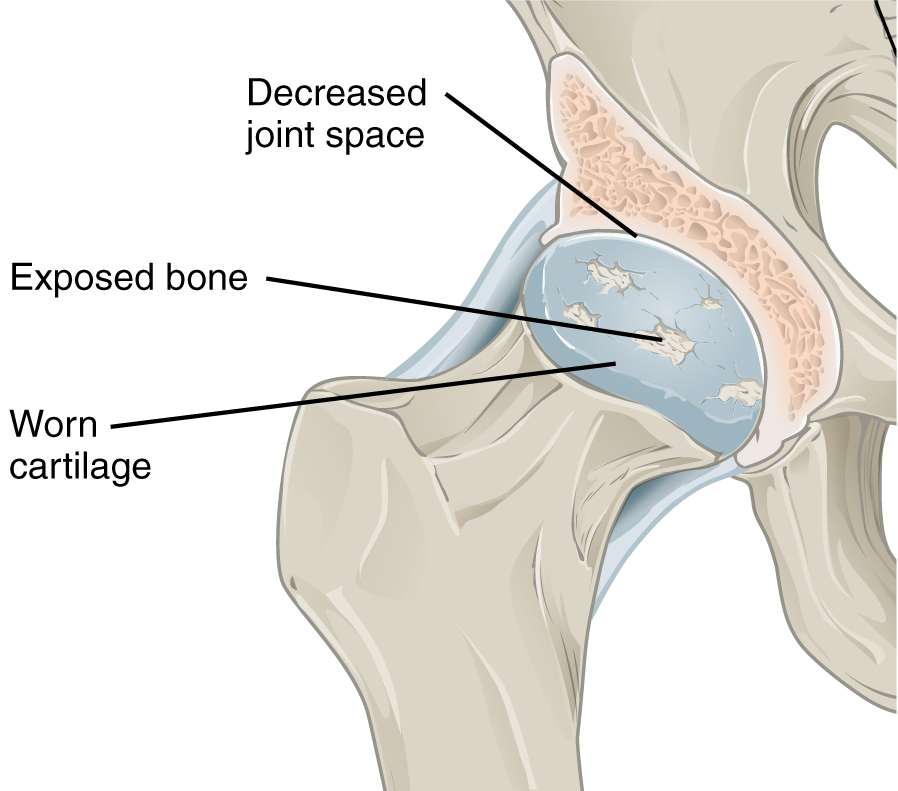
Pathophysiology
There are several structures around the hip that are richly innervated by sensory nerve fibres. These include the periosteum, subchondral bone, synovium, and surrounding soft tissues. In the presence of Central Sensitisation there may be an additional central physiological process. Hip osteoarthritis can also lead to changes in gait which can lead to pain in the knees and lumbar spine.[3]
Higher bone density can drive knee osteoarthritis but not hip osteoarthritis
Clinical Features
History
The pain is often poorly localised. Patients can have pain over quite a large area including the front of the thighs, groin, lateral thighs, buttocks, and the posterior upper thighs. Patients with Central Sensitisation can have unusual distributions of pain at a surprising distance from the hip such as below the knee.
There is no clear association between pain levels and radiographic severity of hip osteoarthritis. Up to 40% of patients with hip osteoarthritis have no pain. Patients with higher pain levels showed differences in sensitisation as measured by quantitative sensory testing.[4]
None of the features on history are particularly helpful on their own for identifying hip OA. Medial thigh pain is highly suggestive of hip OA but is only present in 2.7% of patients. The presence of morning stiffness, pain on walking, and relief of pain on sitting all have positive likelihood ratios of <2.0, but their negative likelihood ratios are more helpful, i.e. the absence of these factors.[3]
| Feature on History | Sensitivity | Specificity | LR+ (95% CI) | LR- (95% CI) |
|---|---|---|---|---|
| Family history of OA | 34% | 84% | 2.1 (1.2-3.6) |
0.79 (0.67-0.93) |
| Personal history of knee OA | 33% | 84% | 2.1 (1.1-3.8) |
0.80 (0.68-0.95) |
| Age > 60 | 96% | 25% | 1.5 (1.3-1.7) |
0.11 (0.02-0.78] |
| Age < 50 | 91% | 28% | 1.3 (1.1-1.5) |
0.32 (0.16-0.62) |
| Worst pain in medial thigh | 12% | 98% | 7.8 (1.7-37) |
0.89 (0.77-1.0) |
| Worst pain in buttock | 12-67% | 57-69% | 0.38-2.0 | 0.38-0.76 |
| Pain on climbing stairs or walking down slopes | 68% | 68% | 2.1 (1.6-2.8) |
0.47 (0.35-0.63) |
| Morning stiffness <60 min | 56-91% | 41-67% | 1.5-1.7 | 0.22-0.65 |
| Pain on initial steps after rest | 92% | 26% | 1.2 (1.1-1.4) |
0.31 (0.08-1.2) |
| Pain on walking | 80-97% | 12-34% | 1.1-1.2 | 0.25-0.58 |
| Pain relieved by sitting | 92% | 33% | 1.4 (0.2-1.6) |
0.24 (0.06-0.92) |
Examination
- Main article: Hip Examination
Physical examination findings are in general more useful than historical features for identifying hip OA. Posterior hip pain is the test with the highest likelihood ratio, but some patients may not be very excited about trying this. Groin pain on hip abduction or adduction, abductor weakness, decreased hip adduction, and decreased hip internal rotation are all findings with positive likelihood ratios above 3. For identifying those who do not have hip OA, normal hip passive adduction or abduction are the most helpful.[3]
Extension is examined with the patient prone and lifting the leg off the table. Flexion is examined with the patient supine, and the examiner lifts the knee to the abdomen. In this position the foot can be kept in the same position, and the knee moved towards the midline, causing internal rotation. The hip can then be moved away from the midline, which causes external rotation. Adduction and abduction are assessed by putting the feet together. The foot is then moved across or away from the midline respectively. Normal ranges of motion are below. Goniometers are sometimes used, but usually estimates are sufficient. The examiner should compare range to the other side, but keeping in mind that osteoarthritis is often bilateral.[3]
| Passive Movement | Normal ROM |
|---|---|
| Flexion | 0 - 140° |
| Internal rotation | 0 - 30° |
| External rotation | 0 - 40° |
| Abduction | 0 - 50° |
| Adduction | 0 - 30° |
| Extension | 0 - 20° |
| Feature on Exam | Sensitivity | Specificity | LR+ (95% CI) | LR-(95% CI) |
|---|---|---|---|---|
| Abductor weakness | 44 | 90 | 4.5
(2.4-8.4) |
0.62
(0.43-0.88) |
| Limp | 85 | 43 | 1.5
(1.2-1.9) |
0.35
(0.20-0.61) |
| Inguinal ligament tenderness | 60 | 75 | 2.4
(1.6-3.8) |
0.53
(0.33-0.87) |
| Tensor fascia lata tenderness | 40 | 80 | 2.0
(1.1-3.4) |
0.75
(0.54-1.1) |
| Squat causing posterior pain | 24 | 96 | 6.1
(1.3-29) |
0.79
(0.62-1.0) |
| Groin pain on abduction or adduction | 33 | 94 | 5.7
(1.6-20) |
0.71
(0.52-0.97) |
| Scour test | 62 | 74 | 2.4
(1.4-4.3) |
0.51
(0.29-0.90) |
| Pain on hip adduction | 68-80 | 46-54 | 1.5 - 1.5 | 0.43-0.59 |
| Pain on hip internal rotation | 82-88 | 38-39 | 1.4 - 1.4 | 0.31-0.45 |
| Restricted movement in 3 planes | NA | NA | 4.4
(2.4-8.3) |
NA |
| Restricted movement in 2 planes | NA | NA | 1.5
(0.90-2.6) |
NA |
| Restricted movement in 1 plane | NA | NA | 1.3
(0.85-2.0) |
NA |
| Restricted movement in 0 planes | NA | NA | 0.91
(0.78-1.1) |
NA |
| Decreased hip adduction | 80 | 81 | 4.2
(3.0-6.0) |
0.25
(0.11-0.54) |
| Decreased hip internal rotation | 66 | 79 | 3.2
(1.7-6.0) |
0.43
(0.31-0.60) |
| Decreased hip range of movement | 75 | 74 | 2.9
(2.1-4.0) |
0.34
(0.25-0.47) |
| Decreased hip extension | 76 | 68 | 2.4
(1.8-3.2) |
0.35
(0.17-0.71) |
| Decreased hip external rotation | 76 | 64 | 2.1
(1.6-2.8) |
0.37
(0.19-0.76) |
| Decreased hip abduction | 88 | 46 | 1.6
(1.3-2.1) |
0.26
(0.09-0.77) |
Combinations of findings have also been studied.
| Findings | Number of findings | LR+ (95% CI) |
|---|---|---|
|
5 or more | 35 (13-95) |
| 4 | 2.0 (0.88-4.3) | |
| 3 or fewer | 0.05 (0.01-0.32) | |
|
4 or more | 4.9 (2.8-8.7) |
| 2-3 | 0.72 (0.57-0.93) | |
| 0 or 1 | 0.24 (0.09-0.64) |
Imaging
Plain radiographs can demonstrate joint space narrowing, osteophytes, subchondral sclerosis, and subchondral cysts. They may also show alternative causes for pain such as pelvic bone tumours.
Laboratory Tests
Depending on the clinical context, rheumatological blood tests may need to be performed.
Diagnosis
The diagnosis can be made clinically in those with mild to moderate symptoms, with examination findings being more useful than historical factors. In those with more severe symptoms then plain radiographs are performed. If the radiographs are normal then there should be a search for other causes of pain.
Plain radiographs are cheap, however because most patients with radiographic OA have asymptomatic disease, there is a risk of incorrectly attributing the pain to osteoarthritis, and subsequently having incorrect treatment. Therefore it is as important as ever to consider the pre-test probability, and consider other diagnoses.
A commonly performed procedure in Musculoskeletal Medicine in New Zealand is the diagnostic intra-articular hip joint injection. Under either ultrasound or fluoroscopic guidance, local anaesthetic is infiltrated into the hip joint. An appreciable reduction in pain post-procedure is consistent with nociception arising from the hip joint.
Differential Diagnosis
- Anterior pain
- Hip Osteoarthritis
- Femoroacetabular Impingement
- Iliopsoas Tendionopathy
- Inflammatory arthritis
- Avascular necrosis/osteonecrosis of the femoral head
- Hip Labral Tear
- Nerve Entrapments: Genitofemoral Nerve Entrapment, Ilioinguinal Nerve Entrapment
- Developmental Dysplasia of the Hip
- Transient Osteoporosis of the Hip
- Inguinal or femoral hernia
- Gynaecological causes
- Gonadal tumours
- Inguinal lymphadenopathy
- Posterior pain
- Lateral pain
- Medial pain
- Other
- Septic Arthritis
- Hip Fracture
- Hip chondral defects
- Ligamentum teres injury
- Pelvic bone tumours
- Pelvic insufficiency fractures
- Stress fracture
- Peripheral Vascular Disease
- Fibromyalgia
- Leaking abdominal aortic aneurysm
Treatment
Research into hip OA has lagged far behind knee OA, and treatment recommendations for hip OA are often extrapolated from knee OA.
Non-pharmacological
Education, exercise, and weight loss are the mainstays of non-pharmacological management of hip and knee osteoarthritis. However long-term compliance is generally challenging.[5]
Some exercise options include aerobic exercise, flexibility exercises, strengthening exercises, water-based exercises, and tai chi. Exercise results in a modest reduction in pain (8 points more than control in a 0-100 scale) and improvement of function (7 points more than control in a 24 point scale).[6] Water-based exercises may be helpful for those with particularly severe symptoms that limit engagement with land-based exercises.
There may be a limited role for physiotherapy over home-exercises, as well as for manual therapy.[7]
The recommendation for weight loss has been extrapolated from knee osteoarthritis and the fact that obesity is a known risk factor for hip osteoarthritis.[8] There are no data on weight loss specifically for reducing symptoms of hip osteoarthritis.\
Medication
NSAIDs are effective for managing hip osteoarthritis, with greater effect with higher doses. Diclofenac 150mg/day is the most effective NSAID available.[9] However, the safety profile needs to be considered for the patient in question, and the lowest dose and shortest duration possible should be used in those with considerable symptoms and poor response to nonpharmacological treatments.
There is no evidence to support single-agent paracetamol.[9]
In a landmark study, opioids were not superior to treatment with nonopioid medications in a study of patients with severe chronic back pain, hip OA, or knee OA.[10] Due to both poor efficacy and safety concerns, opioids should not generally be used for hip osteoarthritis.
Injections
- Main article: Hip Joint Injection
Hip joint steroid injections have a moderate short term effect for up to 8 weeks, and are generally well tolerated. The quality of the evidence however is generally poor.[11] The author is more likely to offer a steroid injection if there is a hip joint effusion. Injections can be done under ultrasound or fluoroscopic guidance.
There is limited evidence to support the use of platelet-rich plasma injections. In recalcitrant disease with the next step being surgery, the author will offer PRP injections into both the hip joint and gluteal tendons, but appreciating that the evidence is poor.
Intra-articular hyaluronic acid injections are no more effective than placebo. The cost of one vial of hyaluronic acid in New Zealand is around $500, and so this treatment has extremely poor cost-effectiveness.[12][13]
Saline appears to be as effective as other options. One systematic review and meta-analysis evaluated saline, glucocorticoids, hyaluronic acid, and PRP, and found that all (except HA+PRP) led to a clinically important improvement in pain.[14]
Surgery
Total hip joint replacement is usually effective for reducing pain. However 10% of patients have chronic postsurgical pain, and preoperative central sensitisation has been thought to be a risk factor for this.[4]
Prognosis
A minority have clear cut clinical and radiological recovery, especially with marked osteophytosis and concentric disease. Superolateral migration of the femoral head is correlated with more rapid osteoarthritis progression, also with atrophic bone response
Resources
- Dieppe PA good author to read
- Media:Hip_Osteoarthritis_-_JAMA_Rational_Clinical_Examination_2019.pdf
References
- ↑ 1.0 1.1 Kim et al.. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: the Framingham osteoarthritis study. Arthritis & rheumatology (Hoboken, N.J.) 2014. 66:3013-7. PMID: 25103598. DOI. Full Text.
- ↑ Iidaka et al.. Prevalence of radiographic hip osteoarthritis and its association with hip pain in Japanese men and women: the ROAD study. Osteoarthritis and cartilage 2016. 24:117-23. PMID: 26241774. DOI.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Metcalfe et al.. Does This Patient Have Hip Osteoarthritis?: The Rational Clinical Examination Systematic Review. JAMA 2019. 322:2323-2333. PMID: 31846019. DOI. Full Text.
- ↑ 4.0 4.1 Hattori T, Shimo K, Niwa Y, Tokiwa Y, Matsubara T. Association of Chronic Pain with Radiologic Severity and Central Sensitization in Hip Osteoarthritis Patients. J Pain Res. 2021;14:1153-1160 DOI
- ↑ Gay et al.. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Annals of physical and rehabilitation medicine 2016. 59:174-183. PMID: 27053003. DOI.
- ↑ Fransen et al.. Exercise for osteoarthritis of the hip. The Cochrane database of systematic reviews 2014. CD007912. PMID: 24756895. DOI.
- ↑ Bennell et al.. Physical therapies in the management of osteoarthritis: current state of the evidence. Current opinion in rheumatology 2015. 27:304-11. PMID: 25775185. DOI.
- ↑ Jiang et al.. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint bone spine 2011. 78:150-5. PMID: 20580591. DOI.
- ↑ 9.0 9.1 da Costa et al.. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: a network meta-analysis. Lancet (London, England) 2017. 390:e21-e33. PMID: 28699595. DOI.
- ↑ Krebs et al.. Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial. JAMA 2018. 319:872-882. PMID: 29509867. DOI. Full Text.
- ↑ McCabe et al.. The efficacy of intra-articular steroids in hip osteoarthritis: a systematic review. Osteoarthritis and cartilage 2016. 24:1509-17. PMID: 27143362. DOI.
- ↑ Brander et al.. Evaluating the use of intra-articular injections as a treatment for painful hip osteoarthritis: a randomized, double-blind, multicenter, parallel-group study comparing a single 6-mL injection of hylan G-F 20 with saline. Osteoarthritis and cartilage 2019. 27:59-70. PMID: 30223023. DOI.
- ↑ Wu et al.. Efficacy of intra-articular hyaluronic acid injections in hip osteoarthritis: a meta-analysis of randomized controlled trials. Oncotarget 2017. 8:86865-86876. PMID: 29156841. DOI. Full Text.
- ↑ Gazendam et al.. Intra-articular saline injection is as effective as corticosteroids, platelet-rich plasma and hyaluronic acid for hip osteoarthritis pain: a systematic review and network meta-analysis of randomised controlled trials. British journal of sports medicine 2021. 55:256-261. PMID: 32829298. DOI.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,