Sacroiliac Joint Pain
The sacroiliac joint is a common source of chronic low back pain. Pain generators are the joint itself, and the surrounding ligaments and muscles. There may be multiple factors coming from the bones, ligaments, muscles, motor control, and alignment.
Anatomy
- Main article: Sacroiliac Joint Anatomy
The sacroiliac joint is a diarthrodial synovial joint, and only the anterior aspect is a true synovial joint. The posterior aspect is a syndesmosis that consists of the gluteus medius, gluteus minimus, sacroiliac ligaments, and piriformis. [1] The anterior joint is thought to be innervated by the ventral rami of L4 and L5, and the posterior joint by the lateral branches of the posterior rami of L5-S4. The superior gluteal nerve contributes.
Epidemiology
The sacroiliac joint accounts for around 16% to 30% of causes of chronic low back pain. Some of the prevalence rates in diagnostic block research are 18% (DePalma 2011), 22.6% (Bernard 1987), 30% (Schwarzer 1995), 18.5% (Maigne 1996), 27% (Irwin 2007), 14.5% (Sembrano 2009).[2]
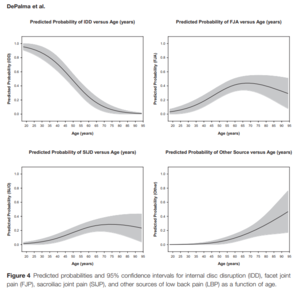
There are three primary groups of patients with sacroiliac joint pain and dysfunction. It occurs post lumbar fusion, in trauma, and in the peripartum. Pain can occur in all age groups from the very young to very old, but there is an increasing rate with age until approximately age 70 when it reverse. The mean age is not significantly different between facetogenic and sacroiliac joint pain, while discogenic pain is more common in younger patients.[2]
In symptomatic post-lumbar fusion patients, the sacroiliac joint is the source of pain about 30-40% of the time. Some of the prevalence rates in this context are 32% (Katz 2003), 35% (Maigne 2005), 43% (DePalma 2001), and 40% (Liliang 2011).[2]
Pathophysiology
- Post-lumbar fusion
Sacroiliac joint pain is almost akin to the idea of adjacent segment degeneration. In the event of L5-S1 fusion, there is 52% added motion on the sacroiliac joint. With L4-S1 fusion there is 168% added motion on the sacroiliac joint. Meanwhile if you fuse the sacroiliac joint, there is only 2-4% added motion on L4 and L5, and 5% added stress on the hip.[3]
- Multi-level fusion
The more spinal levels that are fused, the higher the stress transfer to the adjacent segment, and the greater the rate of sacroiliac joint pain post-operatively. Rates are 5.8% (1 segment fused), 10% (2 segments), 20% (3 segments), and 22.5% (4+ segments).[3][4]
- Trauma
A very common cause of sacroiliac joint pain is a rear-end accident. The mechanism is from hitting the brake, getting hit from the back with an extended leg, and the leg gets forced back. Another common mechanism is missing a step, with force transmission right up the leg to the side. It can also occur with falling on the buttock, and twisting.
Clinical Assessment
There are many challenges with diagnosis, relating to the clinical assessment, imaging studies, and precision diagnosis.
Firstly Sacroiliac joint symptoms overlap with lumbar spine and hip pain symptoms. Sacroiliac joint pain is typically felt a bit lower than for discogenic and facetogenic pain, but there is significant overlap. There may be somatic referred pain down the leg, and into the groin, but is not normally as prominent. Hip joint pain can very commonly cause posterior pain, with the most common patterns in descending frequency: Buttock and thigh, buttock and groin, buttock alone, groin alone, and groin and thigh.[5][2]
Another difficulty is that imaging studies are often inconclusive, and there may not be degenerative changes in proven cases of sacroiliac joint pain.
History
It is important to get details of any prior trauma, spinal fusion, and pregnancy history. See the pathophysiology section above.
Commonly painful movements are ascending/descending stairs, transitional movements (e.g. sitting to stand, supine to sitting), and rolling over in bed. Other painful movements are getting in/out of bed, sitting on the affected side, and prolonged sitting/standing.[6]
Common relieving factors are bearing weight on the unaffected side, lying on the unaffected side, and manual or belt stabilisation.[6]
Examination
- Main article: Sacroiliac Joint Examination
Complete inspection, palpation, range of motion, gait, and neurological tests.
The "Fortin finger test" is a test of pointing within 1cm inferomedial of the PSIS, consistent over at least 2 trials (e.g. beginning and end of exam). If the pointed area is below L5 then consider the sacroiliac joint. If it is above L5 then consider lumbar spine aetiology.[7] Tenderness over the PSIS and sacral sulcus may be a good indicator of a pain source.
It is very important to do a hip examination. Examine FABER (pain anterior for intra-articular hip pathology), Scour (for hip OA and other pathologies), and FADIR (for FAI and labral tears).
Do a single leg stance, functional testing (stairs, sit to stand), active straight leg raise, and provocative testing. There may be a lurching and hobbling gait.
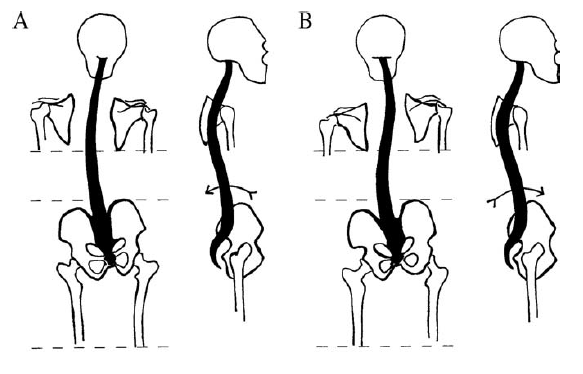
Pelvic Malalignment
Timgren et al assessed pelvic asymmetry in neurologic patients with symptoms that weren't explained by a neurological diagnosis. They found pelvic asymmetry in 87%. Reestablishment and maintenance of symmetry correlated with improvement in pain and function. An average of 3.7 appointments was needed. They found the following patterns. [8]
| Innominate | A. Posterior rotation | B. Anterior Rotation |
|---|---|---|
| Iliac Crest | Elevated ↑ | Elevated ↑ |
| ASIS | Elevated ↑ | Depressed ↓ |
| PSIS | Depressed ↓ | Elevated ↑ |
| scapula | Depressed ↓ | Elevated ↑ |
| leg | Longer ↑ | Shorter ↓ |
| 10-15mm lift | Increased crest difference ↑ | Reduced crest difference ↓ |
| Spinal curvature | C type scoliosis | S type scoliosis |
| C0-C1 function | Symmetric rotation in flexion | Restricted rotation in flexion |
All changes are in reference the ipsilateral side.
Rising of the crest upon anterior SI rotation is paradoxical, and its explanation cannot be reduced to a two-dimensional model.
Schamberger’s rule of the five Ls, which relates to the side of the anteriorly rotated innominate: “Leg Lengthens Lying, Landmarks Lower” (supine vs long sitting) [9]
Diagnosis
The main differentials are hip pain, discogenic pain with or without radicular pain, and facetogenic pain, as per the clinical assessment section above.
- Sacroiliac ligament pain (interosseous or dorsal ligaments)
- Mechanical
- Locking
- Hypermobility
- Osteoarthritis
- Following Lumbosacral fusion
- Fracture
- Tumour
- Rheumatological disorders
- Axial spondyloarthritis
- Psoriatic arthritis
- Infection
- Myofascial pain (Quadratus Lumborum, Gluteus Maximus, Piriformis, Levator Ani)
- Secondary causes: Discogenic pain, Facet joint pain, Hip disease, Spinal stenosis, Flail coccyx (coccydynia), S1 foraminal stenosis
Treatment
Manual therapy may be the most effective initial treatment modality. In a single blind randomised trial of 51 patients with sacroiliac joint related back and leg pain, 56% were successfully treatment. Physiotherapy was successful in 3 out of 15 (20%), manual therapy in 13 out of 18 (72%), and intra-articular injections in 9 out of 18 (50%). Manual therapy consistent of two sessions of high-velocity thrust SIJ manipulation with an interval of 2 weeks. The injection arm was a fluoroscopically guided lidocaine and triamcinolone injection. [10]
Manual Therapy
Alignment can be reacquired through various means such as muscle energy techniques, and mobilisation with movement.
Mulligan Techniques
- Anterior Innominate Rotation
The most common malalignment is anterior rotation. This can usually be easily corrected with a mobilisation with movement technique called anterior innominate extension in lying mobilisation with movement. The sacrum is stabilised, the innominate is rotated and glided posteriorly, while the patient extends in lying. Ensure mobilisation is a combination of glide +/- rotation of the innominate with opposing forces on the sacrum. This technique often corrects posterior rotation, too.
- Mulligan Videos
Muscle Energy Techniques
Pelvic asymmetries can also be corrected with muscle energy techniques.
- Anterior Innominate Rotation
The technique can be visualised via the image below where the origin and insertion of the hamstrings are reversed to pull and rotate the innominate. Ensure to lean cranially, and allow some abduction of the ipsilateral hip. Stabilise the contralateral ASIS. Reach the end range of hip flexion and complete a muscle energy technique. The patient can treat themselves by grasping under their knees and resisting thigh extension, alternating on both sides. This again produces a correctional rotational force on the pelvis.
HVLA techniques
High-velocity and low-amplitude thrust technique can be applied through the ankle on the side of the dysfunctional SI joint
Precision Treatment
- Main article: Sacroiliac Joint Precision Treatment
The sacroiliac joint can treated with radiofrequency neurotomy after a confirmatory single or dual diagnostic block. Cooled radiofrequency neurotomy has an evidence base, while traditional radiofrequency does not.
Article Downloads
References
- ↑ Vanelderen et al.. 13. Sacroiliac joint pain. Pain practice : the official journal of World Institute of Pain 2010. 10:470-8. PMID: 20667026. DOI.
- ↑ 2.0 2.1 2.2 2.3 2.4 DePalma et al.. What is the source of chronic low back pain and does age play a role?. Pain medicine (Malden, Mass.) 2011. 12:224-33. PMID: 21266006. DOI.
- ↑ 3.0 3.1 Ivanov et al.. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine 2009. 34:E162-9. PMID: 19247155. DOI.
- ↑ Unoki et al.. Fusion of Multiple Segments Can Increase the Incidence of Sacroiliac Joint Pain After Lumbar or Lumbosacral Fusion. Spine 2016. 41:999-1005. PMID: 26689576. DOI.
- ↑ Lesher et al.. Hip joint pain referral patterns: a descriptive study. Pain medicine (Malden, Mass.) 2008. 9:22-5. PMID: 18254763. DOI.
- ↑ 6.0 6.1 Janda V. On the concept of postural muscles and posture in man. Aust J Physiotherapy. 1983;29:83-90
- ↑ Fortin & Falco. The Fortin finger test: an indicator of sacroiliac pain. American journal of orthopedics (Belle Mead, N.J.) 1997. 26:477-80. PMID: 9247654.
- ↑ Timgren & Soinila. Reversible pelvic asymmetry: an overlooked syndrome manifesting as scoliosis, apparent leg-length difference, and neurologic symptoms. Journal of manipulative and physiological therapeutics 2006. 29:561-5. PMID: 16949945. DOI.
- ↑ Wolf Schamberger. The Malalignment Syndrome 2nd Edition. Churchill Livingstone. 2012
- ↑ Visser et al.. Treatment of the sacroiliac joint in patients with leg pain: a randomized-controlled trial. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2013. 22:2310-7. PMID: 23720124. DOI. Full Text.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,