Acute Low Back Pain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 14: | Line 14: | ||
Acute pain is pain that has been present for no longer than 12 weeks. Subacute pain is pain present for longer than 5 or 7 weeks but less than 12 weeks. The management differs depending on the acuity. | Acute pain is pain that has been present for no longer than 12 weeks. Subacute pain is pain present for longer than 5 or 7 weeks but less than 12 weeks. The management differs depending on the acuity. | ||
== Referred Pain == | |||
{{Main|Low_Back_Pain_Definitions#Referred_Pain}} | |||
[[Referred Pain|Referred pain]] is "pain perceived as arising or occurring in a region of the body innervated by nerves or branches of nerves other than those that innervate the actual source of pain" | |||
[[Visceral Pain|Visceral referred pain]] is referred pain where the source lies in an organ or blood vessel of the body. With low back pain, the uterus and abdominal aorta are important considerations. Other viscera with higher segmental supply may cause back pain such as pancreatitis, but this may be due to irritation of the posterior abdominal wall, in which case the pain is not truly referred in nature. | |||
[[Somatic Referred Pain|Somatic referred pain]] is referred pain where the source originates in a tissue or structure of the body wall or limbs. A number of structures in the lumbar spine are capable of nociception including the lumbar zygapophysial joints, intervertebral discs, sacroiliac joints, and more. | |||
[[Lumbar Radicular Pain|Radicular pain]] is a subset of [[Neuropathic Pain|neuropathic pain]], and refers to pain that is evoked with stimulation of the nerve roots or dorsal root ganglion of a spinal nerve. In radicular pain, the pain is felt in the peripheral innervation of the affected nerve. | |||
It is important to distinguish somatic referred from radicular pain. Incorrectly distinguishing radicular pain from somatic referred pain is a common pitfall in diagnosis and with incorrect diagnosis this frequently leads to incorrect treatment. | |||
{| class="wikitable" | |||
|+Somatic Referred vs Radicular Pai<span class="reference" id="cite_ref-:0_3-2"></span>n | |||
! | |||
!Somatic Referred | |||
!Radicular | |||
|- | |||
|Pain distal to the knee | |||
|Can occur | |||
|Can occur | |||
|- | |||
|Pain quality | |||
|Dull, deep ache, or pressure-like | |||
|Shooting, lancinating, or electric | |||
|- | |||
|Distribution | |||
|Distributed in wide areas, with difficult to perceive boundaries. The centres in contrast can be confidently indicated. | |||
|Distributed along a narrow band, no more than 2 inches wide | |||
|- | |||
|Traveling | |||
|Fixed in location. It can feel like an expanding pressure into the lower limb, but remains in location once established without traveling. It can wax and one, but does so in the same location. | |||
|Travels into the lower limb | |||
|} | |||
== Aetiology == | == Aetiology == | ||
| Line 49: | Line 83: | ||
*Use of intravenous drugs or steroids, substance abuse or immunosuppression (fracture, infection) | *Use of intravenous drugs or steroids, substance abuse or immunosuppression (fracture, infection) | ||
*Patient aged over 50 years with first episode, and especially age over 65 years (osteoporotic fracture, cancer)}} | *Patient aged over 50 years with first episode, and especially age over 65 years (osteoporotic fracture, cancer)}} | ||
== Management == | |||
Because a specific tissue diagnosis cannot be made with any validity in the vast majority of cases of acute low back pain, the management is not based on finding and treating a particular cause. | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Presenting Complaints]] | [[Category:Presenting Complaints]] | ||
[[Category:Lumbar Spine]] | [[Category:Lumbar Spine]] | ||
Revision as of 18:40, 29 August 2021
Biomedically there are three aims in the approach to acute low back pain. The first is to determine whether the presenting complaint is in fact low back pain, and whether it is acute or not. The second aim is to determine whether any referred pain is somatic referred pain or radicular pain. The third aim is to identify any serious conditions.[1]
Definitions
- Main article: Low Back Pain Definitions
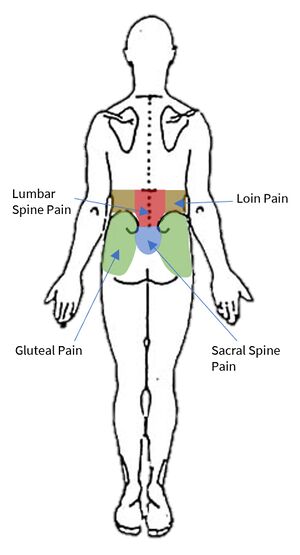
Starting with the wrong definition of low back pain can lead to the wrong diagnosis, and so it is important to be clear here. The IASP taxonomy categorises low back pain into lumbar spinal pain and sacral spinal pain. There is also an overlapping definition called lumbosacral pain. These three categories constitute the colloquial term "low back pain."
Lumbar spinal pain is pain in a region bounded superiorly by an imaginary transverse line through the tip T12, inferiorly by an imaginary transverse line through the tip of S1, and laterally by vertical lines tangential to the lateral borders of the lumbar erectores spinae.
Sacral Spinal Pain is pain in a region bounded superiorly by an imaginary transverse line through the tip of S1, inferiorly by an imaginary transverse line through the posterior sacrococcygeal joints, and laterally by imaginary lines passing through the posterior superior and posterior inferior iliac spines."
Lumbosacral Pain is pain perceived as arising from a region encompassing or centred over the lower third of the lumbar region as described above and the upper third of the sacral region as described above.
Acute pain is pain that has been present for no longer than 12 weeks. Subacute pain is pain present for longer than 5 or 7 weeks but less than 12 weeks. The management differs depending on the acuity.
Referred Pain
- Main article: Low_Back_Pain_Definitions#Referred_Pain
Referred pain is "pain perceived as arising or occurring in a region of the body innervated by nerves or branches of nerves other than those that innervate the actual source of pain"
Visceral referred pain is referred pain where the source lies in an organ or blood vessel of the body. With low back pain, the uterus and abdominal aorta are important considerations. Other viscera with higher segmental supply may cause back pain such as pancreatitis, but this may be due to irritation of the posterior abdominal wall, in which case the pain is not truly referred in nature.
Somatic referred pain is referred pain where the source originates in a tissue or structure of the body wall or limbs. A number of structures in the lumbar spine are capable of nociception including the lumbar zygapophysial joints, intervertebral discs, sacroiliac joints, and more.
Radicular pain is a subset of neuropathic pain, and refers to pain that is evoked with stimulation of the nerve roots or dorsal root ganglion of a spinal nerve. In radicular pain, the pain is felt in the peripheral innervation of the affected nerve.
It is important to distinguish somatic referred from radicular pain. Incorrectly distinguishing radicular pain from somatic referred pain is a common pitfall in diagnosis and with incorrect diagnosis this frequently leads to incorrect treatment.
| Somatic Referred | Radicular | |
|---|---|---|
| Pain distal to the knee | Can occur | Can occur |
| Pain quality | Dull, deep ache, or pressure-like | Shooting, lancinating, or electric |
| Distribution | Distributed in wide areas, with difficult to perceive boundaries. The centres in contrast can be confidently indicated. | Distributed along a narrow band, no more than 2 inches wide |
| Traveling | Fixed in location. It can feel like an expanding pressure into the lower limb, but remains in location once established without traveling. It can wax and one, but does so in the same location. | Travels into the lower limb |
Aetiology
Unlike with chronic low back pain there is little research on the aetiology of acute low back pain. No patho-anatomic diagnosis of low back pain can be made clinically without the use of special investigations (e.g. discography, medial branch blocks, sacroiliac joint blocks). Special investigations are not appropriate for acute low back pain, and are reserved for chronic low back pain. Furthermore medical imaging is not able to identify sources of pain other than fractures.
The most important part of the assessment in acute low back pain is evaluating for red flag conditions. Fractures occur between 1-4% of cases, malignancy in 0.2%, and infection in 0.01%. Other conditions that are important to detect are cauda equina, and spondyloarthropathies.[1]
In the acute setting in the absence of red flags, the diagnosis is simply "acute low back pain."[2]
Prognosis
- Main article: Prognosis of Low Back Pain
It is sometimes stated in guidelines that most patients with acute low back pain make an excellent recovery. The evidence is in fact quite conflicting, with markedly different findings across different studies. Overall the treating doctor can relay optimism, but be guarded about prognosis. The data on recurrence rates are also conflicting.
A systematic review of 11 studies performed in the US, Australia and Europe on patients with non-specific back pain found that recovery occurred in 33% of patients at 3 months, and by 1 year 65% still had pain. In studies that used total absence of pain as a criterion, 71% still had pain at 12 months. In studies that had a less stringent criteria, 57% still had pain at 12 months.[3]
Prognostic risk factors are broadly categorised into biological and psychosocial. Predictors of recurrence are often variable across studies, but generally include [4][5]
- Sociodemographic: female gender, obesity, poor educational level
- Current History: previous episodes, duration of episode, days to seek care, pain and disability levels, leg pain
- General Health: Smoking, habitual physical activity, perceived health, use of medications
- Psychosocial: Perceived risk of recurrence, depression, anxiety, fear-avoidance behaviour, overprotective family or lack of support.
- Work-related: Involvement in heavy lifting or awkward positions, job satisfaction, compensable case
- Others: MRI findings, qualification of practitioner.
The psychosocial and occupational barriers are termed "yellow flags".
Assessment
- Signs or symptoms of cauda equina syndrome (e.g. bladder or bowel dysfunction, altered sensation in saddle area)
- Progressive or persistent neurological (motor or sensory) deficit or widespread neurological signs (cauda equina, cancer)
- Severe worsening or unremitting pain, especially at night or worse when lying down (cancer, infection)
- History of significant spinal pathology or osteoporosis (fracture, specific spinal pathology)
- Significant trauma or penetrating wound near spine (fracture, infection)
- Unexplained weight loss (cancer)
- History of cancer or suspicion of recurrent cancer
- Fever, chills, recent urinary tract or skin infection
- Use of intravenous drugs or steroids, substance abuse or immunosuppression (fracture, infection)
- Patient aged over 50 years with first episode, and especially age over 65 years (osteoporotic fracture, cancer)
Management
Because a specific tissue diagnosis cannot be made with any validity in the vast majority of cases of acute low back pain, the management is not based on finding and treating a particular cause.
References
- ↑ 1.0 1.1 Wade King and Nikolai Bogduk. Acute Low Back Pain. Bonica's Management of Pain. 2018
- ↑ Bogduk et al. Medical Management of Acute and Chronic Low Back Pain. Chapter 3. Elsevier 2002.
- ↑ Itz CJ, Geurts JW, van Kleef M, Nelemans P. Clinical Course of Non-Specific Low Back Pain: A Systematic Review of Prospective Cohort Studies Set in Primary Care. Eur J Pain. 2013;17(1):5-15. doi: 10.1002/j.1532-2149.2012.00170.x.
- ↑ Machado GC, et al. Can Recurrence After an Acute Episode of Low Back Pain Be Predicted? Phys Ther. 2017 Sep 1;97(9):889-895. doi: 10.1093/ptj/pzx067. PMID: 28969347
- ↑ National Health Committee. Low Back Pain: A Pathway to Prioritisation. 2015. Full Text