Sacroiliac Joint Injection: Difference between revisions
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
}} | }} | ||
[[Sacroiliac Joint Pain|Sacroiliac joint pain]] is common, and the structure is the source of pain in 16-30% of cases of chronic low back pain. See [[Sacroiliac Joint Precision Treatment]] for more information about precision treatments for this structure. | [[Sacroiliac Joint Pain|Sacroiliac joint pain]] is common, and the structure is the source of pain in 16-30% of cases of chronic low back pain. The area can be injected at the bedside, but the gold standard is fluoroscopic guidance. See [[Sacroiliac Joint Precision Treatment]] for more information about precision treatments for this structure. | ||
==Anatomy== | ==Anatomy== | ||
Revision as of 13:17, 23 August 2020
| |
| Sacroiliac Joint Injection | |
|---|---|
| Indication | Sacroiliac joint pain or dysfunction, sacroiliitis / ankylosing spondylitis, SIJ arthritis |
| Needle | 21gauge 70mm needle |
| Steroid | optional 40mg triamcinolone |
| Volume | The joint can take approximately 2mL |
Sacroiliac joint pain is common, and the structure is the source of pain in 16-30% of cases of chronic low back pain. The area can be injected at the bedside, but the gold standard is fluoroscopic guidance. See Sacroiliac Joint Precision Treatment for more information about precision treatments for this structure.
Anatomy
- Main article: Sacroiliac Joint Anatomy
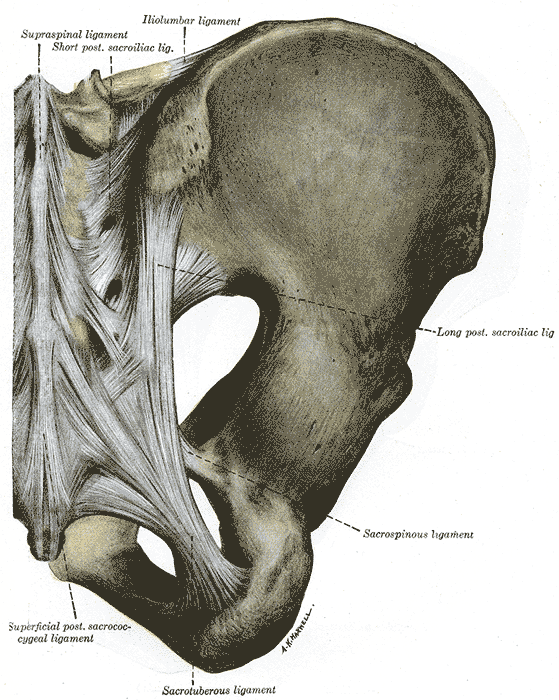
The sacroiliac joint is around 1-2mm wide and is formed within S1, S2, and S3. The concave sacral surface joins with the convex ilium surface. The joint has an interlocking mechanism due to an irregular sacral surface. The capsule is often indistinguishable from the surrounding ligaments. The strongest ligament is the interosseous ligament. Other ligaments are the anterior and posterior sacroiliac ligaments, the sacrotuberous ligament which attaches to the coccygeal vertebrae and the ischial tuberosity, and the sacrospinous ligament which joins the ischial spine to the sacrum and coccyx. The anterior joint is thought to be innervated by the ventral rami of L4 and L5, and the posterior joint by the lateral branches of the posterior rami of L5-S4. The superior gluteal nerve contributes.
Indications
Diagnostic block for sacroiliitis / ankylosing spondylitis, SIJ arthritis, SIJ dysfunction, gout, rheumatoid arthritis, psoriasis, congenital deformity
Contraindications
Relative contraindications: Bleeding diatheses, fracture, malignancy
Technique
Ultrasound Guided
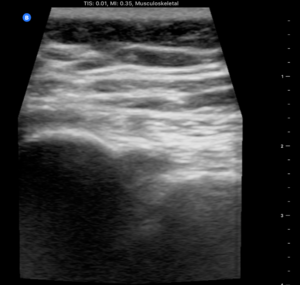
USS has been shown to have up to 90% success rate[1] and even if not intraarticular then USS ensures peri-articular injection which is believed to be effective.[2]
Landmarks: Patient in prone position. Bony landmarks of PSIS, spinous process L5.
USS landmarks: probe in transverse/axial view from L5, down to the sacral median crest. Probe then goes lateral over the sacrum until the PSIS is visible. The notch in between represents the joint in an axial view. The dorsal SIJ ligaments should be visible connecting the sacrum to the ilium.
Mark out the probe position with permanent marker.
Wipe down area, sterile field: skin prep, sterile jelly, sterile probe.
- Needle placement
- Medial to lateral approach: place probe in position then needle enters skin in midline - approximately 2cm from the heel of the probe and has a shallow trajectory towards probe. Needle tip will appear in joint when under the middle of the probe.
- Caudal to cranial approach: The other option is to enter the needle caudally to the marker on the probe and aim cranially and laterally (15deg) until needle tip enters joint in the midline of the probe. The ultrasound probe placement for this approach is shown in the attached video in the video section.
Local anaesthetic: 27gauge needle USS guidance around and on top of the dorsal ligaments.
Corticosteroid: 21gauge 70mm needle into joint and inject. Note the tactile sensation of pushing through leather then the release once in joint. Joint can take up to 2mm of steroid then will feel resistance.
Landmark Guided
This is not recommended. You can inject the dorsal sacroiliac ligaments but not the joint itself without ultrasound or fluoroscopic guidance. Because of the obliquity of the three dimensional anatomy blind injection is often unsuccessful [2]
Complications
Infection - risk 1:10,000. Fatty atrophy. Skin depigmentation. Risks mitigated if sterile field and steroid not injected subcutaneously.
Aftercare
Post procedure: dressings, icepack, education, exercises, pain diary.
Videos
See Also
External Links
References
- ↑ Klauser et al.. Feasibility of ultrasound-guided sacroiliac joint injection considering sonoanatomic landmarks at two different levels in cadavers and patients. Arthritis and rheumatism 2008. 59:1618-24. PMID: 18975358. DOI.
- ↑ 2.0 2.1 Hartung et al.. Ultrasound-guided sacroiliac joint injection in patients with established sacroiliitis: precise IA injection verified by MRI scanning does not predict clinical outcome. Rheumatology (Oxford, England) 2010. 49:1479-82. PMID: 20019067. DOI.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,