Nonsteroidal Anti-Inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) are members of a drug class that inhibit the activity of cyclooxygenase (COX-1 or COX-2) enzymes. This confers them analgesic, antipyretic, and anti-inflammatory effects, as well as inhibition of platelet aggregation. Side effects depend on the specific drug but largely include an increased risk of gastrointestinal ulcers and bleeds, heart attack, and kidney disease.
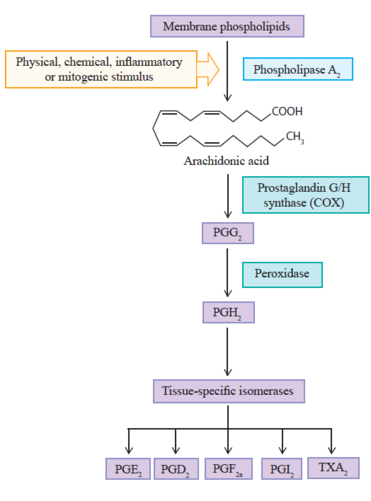
Prostanoid Biosynthesis
Biosynthesis starts with arachidonic acid which is present in the lipid bilayer of the cell membrane. The biosynthesis pathway has three main steps.
Initially arachidonic acid is liberated, by hydrolysis, by phospholipase A2 enzyme (PLA2). The second step involves the COX enzyme, through its cyclooxygenase site, which results in prostaglandin G2 (PGG2). The same COX enzyme converts PGG2 to prostaglandin H2 (PGH2) through the COX peroxidase catalytic site.
PGH2 is converted to various kinds of prostanoids by tissue-specific isomerases. For example prostacyclin (PGI2), prostaglandin D2 (PGD2), prostaglandin E2 (PGE2), prostaglandin F2a (PGF2a) and thromboxane A2 (TXA2).
One end of the COX enzyme has a membrane binding domain along with an epithelial growth factor domain, and the other end is the active enzymatic site.
COX Enzymes
There are different COX isoforms, but the most studied are COX-1 and COX-2. They differ only in the amino acid at site 523 with COX1 having isoleucin, and COX2 having valine. Both COX isoenzymes act on arachidonic acid, but the difference lies in genes that produce them and the factors that trigger those genes.
COX-1
COX-1 is a "housekeeping" enzyme that is constantly expressed in nearly all tissues such as platelets, gastrointestinal tract, kidney, endothelium, uterus, and brain.
It is involved in the mediation of physiological responses through maintaining a basal rate of prostanoids in the tissues. For example is involved in cytoprotection of the stomach, platelet aggregation, and facilitating blood flow through tissues especially the stomach and kidney.
COX-2
Traditionally COX-2 was thought to only be expressed by cells involved in inflammation such as macrophages, monocytes, and synoviocytes. The expression is triggered by tissue damage in order to promote repair. The production of COX-2 increases by 20 times in the presence of inflammatory stimuli, and so it is the primary enzyme that is responsible for the synthesis of prostanoids in acute and chronic pathological inflammatory states.
This is however an overly simplified view. COX-2 is not an exclusively proinflammatory inducible enzyme. It is basally expressed in many organs such as the ovary, uterus, brain, spinal cord, kidney, cartilage, bone, and the gastrointestinal tract. It plays a more complex physiological role than previously recognised. For example, in the kidney it is responsible for ensuring tubuloglomerular feedback.
The expression is regulated by several mediators e.g. lipopolysaccharide, proinflammatory cytokines, and growth factors. Glucocorticoids inhibit COX-2 expression.
Prostaglandins
Prostaglandin H2 (PGH2) has its own actions or can be converted to other prostaglandins such as PGE2, PGI2, PGD2, PGF2a, and TXA2.
- PGE2produces fever, vasodilation with resulting lowering of blood pressure and promoting blood flow to the kidney and gastrointestinal tract, diuresis, and in the uterus it causes smooth muscle contraction.
- PGH2increases blood pressure, i.e. it competes against PGE2.
- PGI2 has the same effects on the gastrointestinal tract as PG2. If fact all PGs have the same effect on the gastrointestinal tract.
- PGI2 inhibits the uterus, i.e. it competes against PGE2
- PGI2 inhibits platelet aggregation, i.e. it competes against thromboxane (TXA2).
- TXA2 promotes platelet aggregation.
Peripheral sensitisation: Prostaglandins regulate the sensitivity of polymodal nociceptors that are present in nearly all tissues. Many of these nociceptors can't be easily activated by physiological stimuli such as light pressure or slight increase in temperature. However, with tissue trauma and the release of prostaglandins, "silent" polymodal nociceptors are able to become excitable to pressure, temperature changes, and acidosis. This results in hyperalgesia and in some cases allodynia. This may be through effects on transient receptor potential vanilloid 1 (TRPV1) in sensory neurons, and tetrodotoxin-resistant sodium channels in dorsal root ganglia. Therefore, at least part of the analgesic action of COX inhibitors is thought to be due to the prevention of peripheral sensitisation.
Central sensitisation: COX-2 expression in the spinal cord may facilitate nociceptive transmission, with prostaglandins acting on the CNS to cause central hyperalgesia. There is widespread induction of COX-2 expression in spinal cord neurons and other regions of the CNS following peripheral inflammation. COX-2 is expressed in the dorsal horn and is upregulated briefly following trauma in the corresponding segment. Prostaglandin E2 has a role in central pain sensitisation. It directly depolarises wide dynamic range neurons into the deep dorsal horn, and reduces the inhibitory tone of the neurotransmitter glycine onto neurons in the superficial layers of the dorsal horn thereby disinhibiting nociceptive transmission.
Pharmacology of NSAIDs
The original NSAIDs operate on locations of the COX enzyme that are identical in both isoenzymes. This results in blocking of both the inflammatory effects of COX2 and the normal physiological effects of COX1. This results in potential side effects particularly on the kidney and stomach.
The COX2-inhibitors bind to a site on COX2 that isn't present or accessible on COX1. which reduces the side effects related to COX1 inhibition.
NSAIDs bind non-competitively to COX, for example ibuprofen. Aspirin on the other hand irreversibly inactivates both COX-1 and COX-2 by acetylating an active-site serine, and this interferes with the binding of arachidonic acid at the active site on COX . This covalent binding means that the antagonistic effects only cease when the receptor or membrane are replaced. Indomethacin, a old NSAID that is no longer available in New Zealand, evolves from non-competitive binding to permanent binding.
COX inhibitors antagonise central hyperalgesia in the dorsal horn through modulating the glutamatergic signalling from nociceptive C fibres to secondary neurons. COX-2 but not COX-1 inhibition suppresses inflammation-induced prostaglandin level rise the CSF.
Paracetamol also deserves special discussion. It was traditionally stated that it acted centrally and was a weak inhibitor of COX-1 and COX-2. It actually acts on both peripheral and central COX enzymes, is a weak anti-inflammatory agent, and has preferential COX-2 inhibition. It acts on COX as a reducing agent within the peroxidase site.
Side Effects
Many of the side effects of NSAIDs are due to COX-1 suppression, such as gastrointestinal ulceration and bleeding, and platelet dysfunction. Selective COX-2 inhibitors were developed with the idea of avoiding the unwanted side effects that are elicited by COX-1 inhibition.
Gastrointestinal Effects
The gastrointestinal side effects are related to direct irritation and reduction of prostaglandin synthesis. Acidic NSAIDs have a topical irritant effect, and because of a phenomenon called "ion trapping" they accumulate in the gastric epithelial cells.
The risk of peptic ulcers in high risk patients can be significantly reduced by the co-administration of a proton-pump inhibitor. However this combination does not protect against damage to the lower gastrointestinal tract.
Cardiovascular Effects
The long term use of both traditional NSAIDs and COX-2 inhibitors confers cardiovascular risks. The mechanism for this relates to the previously unrecognised role of COX-2 expression in basal conditions, and the blockade of COX-2 dependent prostaglandins such as prostacyclin. Prostacyclin is reduced by over 60% by both traditional NSAIDs and COX-2 inhibitors. Prostacyclin is a potent inhibitor of platelet aggregation, and also plays a role in hypertension, atherogenesis, and cardiac dysfunction.
The differential profile of cardiovascular side effects of NSAIDs and COX-2 inhibitors may be related to degree and time course of intravascular COX-2 inhibition. It was previously thought that COX-1 inhibition was protective due to inhibition of platelet aggregation, but this effect only occurs with suppression of >95% of COX-1 activity. This is only seen with low-dose aspirin and in some people with naproxen dosed at 500mg twice daily.
Refecoxib (Vioxx) and valdecoxib (Bextra) were withdrawn from the market due to the increased number of severe thromboembolic events with short term treatment. This has resulted in the change in labelling of all COX inhibitors to encourage taking them at the lowest effective dose for the shortest possible duration.
Ibuprofen and diclofenac, but not naproxen also confer an increased risk for vascular events. The rate of serious vascular events is similar to COX-2 inhibitors and any non-naproxen NSAID.
Renal Effects
COX-2 is also involved in renal function, and so NSAIDs and COX-2 inhibitors can also cause peripheral oedema, hypertension, and inhibition of water and salt excretion leading to exacerbation of hypertension.
Asthmatics
COX-1 inhibition is also the mechanism for aspirin hypersensitivity and unrelated NSAIDs in some patients with asthma and in some patients with chronic urticaria-angioedema. In these cases, COX-1 inhibition results in activation of the lipoxygenase pathway which induces bronchospasm and nasal obstruction.
In accordance with the role of COX-1 in aspirin-induced asthma, COX-2 inhibitors tend to be well tolerated by patients as shown in several re-exposure studies. However the product information sheets still lists this as a contraindication.
Different NSAIDs
Nomenclature
The naming scheme of NSAIDs is related to the base molecule from which they are derived.
- pyrroleACetic - diclofenAC, ketorolAC
- PROpionic - ibuPROfen, naPROxen
- sALicylates - acetylesALicylic acid
- OXycams - pirOXicam
- indoleACetic - indomethACin
Comparisons
| Drug | Chemical Subclass | pKa | Plasma
protein binding |
Oral bioavailability | t-max† | Half life | Single dose
(maximal daily dose) for adults |
Side Effects (SEs) |
|---|---|---|---|---|---|---|---|---|
| Low potency / short elimination half life compounds | ||||||||
| Aspirin | Salicylates | 3.5 | 50-70% | ~50%, dose dependent | ~15 min | ~15 min** | 0.05-1g (~6g)‡ | Long lasting platelet effect. GIT SEs. Reye's syndrome in children. |
| Ibuprofen | 2-Arylpropionic acids | 4.4 | 99% | 100% | 0.5-2h | 2h | 200-800mg (2.4g) | High doses has increased GIT SEs. CVD RR 1.51[1] |
| Mefenamic acid | Anthranilic acids | 4.2 | 90% | 70% | 2-4h | 1-2h | 250-500mg (1.5g) | |
| High potency / short elimination half life compounds | ||||||||
| Diclofenac | Aryl-/heteroarylacetic acids | 3.9 | 99.7% | ~50%, dose dependent,
high first pass metabolism |
1-12h, variable | 1-2h* | 25-75mg (150mg) | Low rate of GIT SEs, slightly higher liver toxicity, CVD RR 1.63[1] |
| Intermediate potency / intermediate elimination half life compounds | ||||||||
| Naproxen | 2-Arylpropionic acids | 4.2 | 99% | 90-100% | 2-4h | 12-15h | 250-500mg (1.25g) | More ulcer bleeds than ibuprofen. CVR RR 0.92[1] |
| High potency / long elimination half life compounds | ||||||||
| Tenoxicam | Oxicams | 5.3 | 99% | ~100% | 0.5-2h | 25-175h¤ | 20-40mg; initial: 40mg | Oxicams have a somewhat higher incidence of GIT and renal effects. |
| Meloxicam | Oxicams | 4.08 | 99.5% | 89% | 7-8h | 20h¤ | 7.5-15mg | |
| Selective COX-2 inhibitors | ||||||||
| Celecoxib | Sulfonamides | 11.1 | 97% | 20 - 60% | 2-4h | 6-12h | 100-200mg (400mg) | Less GIT SEs∞. Increased CVD SEs. |
| Etoricoxib | Methylsulfons | 4.96 | 92% | ~ 100% | 1h | 20-26h | 120mg | Similar CVD SEs to diclofenac. |
| Paracetamol | ||||||||
| Paracetamol | Aniline derivatives | 5-50% | 70 - 100% | 70 - 100%, dose dependent | 0.5-1.5h | 1.5-2.5h | 0.5-1g (4g) | Less GIT SEs. Similar CVD SEs. Dose dependent hepatotoxicity. |
|
† Time to reach maximum plasma concentration Modified from Pharmacology of Cyclooxygenase Inhibitors. Encyclopedia of Pain 2013.[2] | ||||||||
See Also
References
- ↑ 1.0 1.1 1.2 Kearney PM, Baigent C, Godwin J, Halls H, Emberson JR, Patrono C. Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials. BMJ. 2006 Jun 3;332(7553):1302-8. doi: 10.1136/bmj.332.7553.1302. PMID: 16740558; PMCID: PMC1473048.
- ↑ Hinz et al. Pharmacology of Cyclooxygenase Inhibitors. Encyclopedia of Pain 2013. Springer, Berlin, Heidelberg.